Hypoglycemia: What It Is, Why It Happens, and How to Prevent It
When your blood sugar drops too low, your body doesn’t just feel tired—it can start shaking, sweating, or even confuse you. This is hypoglycemia, a condition where blood glucose falls below 70 mg/dL, triggering physical and neurological symptoms. Also known as low blood sugar, it’s not just a side effect of diabetes—it’s a real emergency that needs quick action. Many people think it only happens to those on insulin, but the truth is, even people taking oral diabetes drugs like sulfonylureas or meglitinides can crash if they skip a meal, over-exercise, or drink alcohol without food.
Diabetes medications, including insulin, glyburide, and glipizide, are the most common cause of hypoglycemia in adults. But it’s not just about the drug—it’s about timing, diet, and activity. A person on insulin might feel fine after breakfast, then crash by mid-afternoon if they didn’t eat enough carbs or took too much dose. Seniors are especially at risk because their bodies don’t bounce back as fast, and they often take multiple meds that can interact. Blood glucose, the amount of sugar circulating in your bloodstream, needs to stay in a narrow range. Too high, and you damage organs over time. Too low, and your brain starts to shut down.
What makes hypoglycemia tricky is that symptoms vary. One person gets dizzy and sweaty. Another feels irritable or confused. Some don’t feel anything at all—a condition called hypoglycemia unawareness, which is especially dangerous. That’s why checking your sugar with a glucometer isn’t optional—it’s lifesaving. And if you’re on a medication that can cause it, you need a plan: always carry fast-acting carbs like glucose tabs, juice, or candy. Tell family or coworkers what to do if you collapse. Keep a glucagon kit handy if you’re on insulin.
The posts below dig into the real-world side of this issue. You’ll find guides on which diabetes drugs are safest for seniors, how to avoid low blood sugar while taking other meds, and what to do when your body stops warning you it’s crashing. There’s no fluff here—just clear, practical advice from people who’ve seen this happen in clinics, homes, and emergency rooms. Whether you’re managing your own sugar or helping someone else, you’ll walk away knowing exactly what to watch for—and how to stop it before it’s too late.

Managing Hypoglycemia from Diabetes Medications: A Practical Step-by-Step Plan
- Dec, 22 2025
- 8
Learn how to prevent and treat low blood sugar caused by diabetes medications. This practical guide covers risk factors, emergency treatment, glucose monitoring, and new technologies to keep you safe.
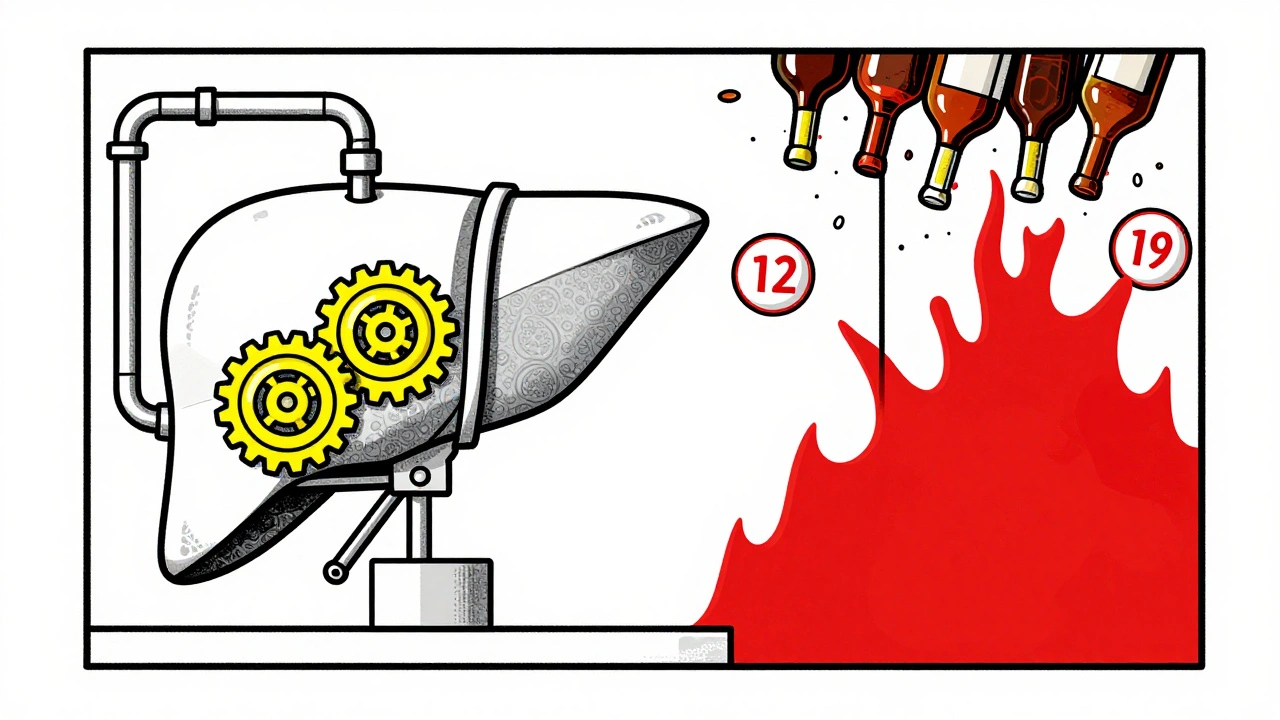
Alcohol and Diabetes Medications: How Drinking Affects Blood Sugar and Liver Health
- Dec, 1 2025
- 8
Drinking alcohol while on diabetes meds can cause dangerous drops in blood sugar and harm your liver. Learn how metformin, insulin, and sulfonylureas interact with alcohol-and what you can do to stay safe.
Categories
- Health and Medicine (63)
- Health and Wellness (57)
- Medicine (37)
- Women's Health (11)
- Mental Health (9)
- Men's Health (7)
- Beauty and Wellness (4)
- Health Information (4)
Archives
- February 2026 (9)
- January 2026 (25)
- December 2025 (28)
- November 2025 (25)
- October 2025 (27)
- September 2025 (14)
- August 2025 (3)
- July 2025 (2)
- June 2025 (2)
- May 2025 (3)
- April 2025 (4)
- March 2025 (4)
- online pharmacy
- medication safety
- dietary supplement
- health benefits
- dietary supplements
- generic drugs
- prevention
- fertility
- online pharmacy Australia
- side effects
- QT prolongation
- medication side effects
- diabetes medications
- GLP-1 agonists
- nocebo effect
- brand vs generic
- treatment
- treatment options
- benefits
- connection
