Alcohol and Diabetes Medications: How Drinking Affects Blood Sugar and Liver Health
 Dec, 1 2025
Dec, 1 2025
Alcohol & Diabetes Risk Assessment Tool
This tool helps you understand risks when drinking alcohol with diabetes medications. Based on article content, never assume alcohol is safe with diabetes meds.
Drinking alcohol while taking diabetes medication isn’t just a bad idea-it can be dangerous. For many people with diabetes, a glass of wine or a beer seems harmless. But when alcohol meets medications like metformin, insulin, or sulfonylureas, it triggers a silent conflict inside the body-one that can drop blood sugar to life-threatening levels or strain the liver beyond repair.
Why Alcohol Causes Low Blood Sugar
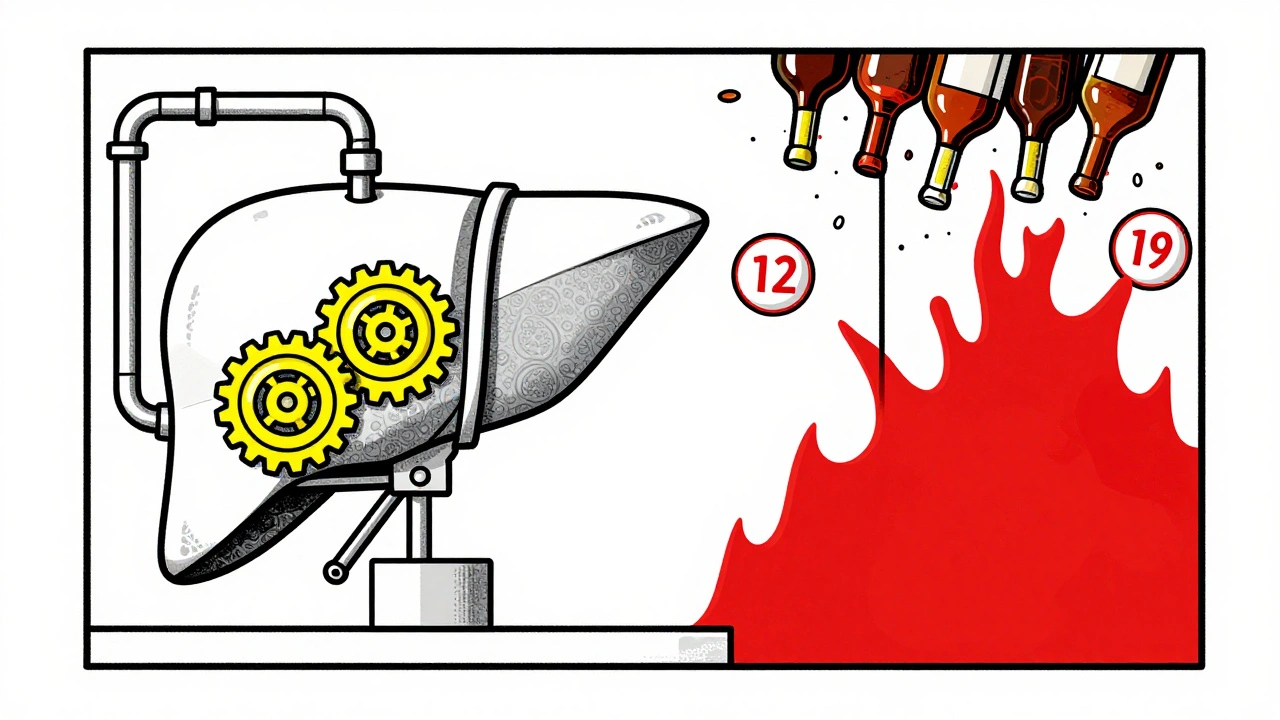
Your liver does two big jobs: it stores sugar when you’ve eaten too much and releases it when you haven’t eaten in a while. That’s how your blood sugar stays steady. But when you drink alcohol, your liver drops everything to deal with the toxin. It stops releasing glucose. And if you’re on medication that pushes your blood sugar down-like insulin or sulfonylureas-your body has no backup.This isn’t just a quick drop. Hypoglycemia can hit hours after your last drink, especially if you’ve been walking, dancing, or exercising. People have woken up in the middle of the night with shaking hands, sweating, and confusion-thinking they’re just hungover. But it’s not a hangover. It’s dangerously low blood sugar.
The scary part? Symptoms of low blood sugar-dizziness, slurred speech, confusion, weakness-look exactly like being drunk. If you pass out after drinking, a friend might assume you’re just passed out from alcohol. They won’t know you need glucose, not more water or coffee. That delay can be deadly.
Metformin and Alcohol: A Risky Mix
Metformin is the most common diabetes pill. It helps your body use insulin better. But it also puts stress on your liver. Alcohol does the same. Together, they overload the organ.When you mix metformin and alcohol, you’re not just increasing the chance of low blood sugar. You’re raising the risk of lactic acidosis-a rare but serious condition where lactic acid builds up in your blood. It happens when the liver can’t clear lactate because it’s busy processing alcohol. Symptoms include nausea, vomiting, stomach pain, muscle cramps, and feeling extremely tired. If you’ve had more than a few drinks and feel this way while on metformin, seek help immediately.
Also, both metformin and alcohol cause stomach upset. Nausea, gas, bloating, and diarrhea are common with metformin. Add alcohol, and those symptoms get worse. Some people stop taking metformin because they think it’s intolerable. But it’s not the drug-it’s the alcohol making it worse.
Insulin and Sulfonylureas: The Highest Risk
If you take insulin or sulfonylureas (like glipizide or glyburide), your risk of hypoglycemia from alcohol is much higher. These medications force your pancreas to release more insulin, whether you need it or not. Alcohol shuts off your liver’s glucose production. The result? Blood sugar plummets with no safety net.People on insulin often report nighttime crashes after drinking. One person on Reddit described setting three alarms after a dinner party-checking blood sugar at 1 a.m., 3 a.m., and 5 a.m. Each time, it was below 70 mg/dL. He ended up drinking juice in bed to stay safe. That’s not unusual. Many users say they’ve needed emergency glucose gel or glucagon shots after drinking, even when they didn’t feel symptoms.
There’s no safe amount for everyone. For some, one drink is enough. For others, it takes three. It depends on your weight, how much you’ve eaten, your liver health, and what meds you’re on. But the rule is simple: if you’re on insulin or sulfonylureas, don’t drink without food-and don’t drink alone.
How Alcohol Affects Your Liver Over Time
Long-term drinking doesn’t just cause one bad night. It damages your liver. Alcohol causes fatty liver, inflammation (hepatitis), and eventually scarring (cirrhosis). All of this makes it harder for your liver to manage blood sugar.People with diabetes already have a higher risk of fatty liver disease. Add alcohol, and the damage speeds up. A damaged liver can’t store sugar properly. It can’t release sugar when needed. It can’t break down medications correctly. That means your diabetes control gets worse. Your meds stop working as well. Your blood sugar swings become wilder.
And it’s not just about the liver. Heavy drinking-defined as more than 15 drinks a week for men or 8 for women-raises your risk of developing type 2 diabetes in the first place. It increases insulin resistance. It raises triglycerides. It adds belly fat. All of this makes diabetes harder to manage, even if you’re not drinking on the same day as your meds.
What to Do If You Choose to Drink
The best advice? Don’t drink. But if you do, here’s how to reduce the risk:- Always eat with alcohol. Have a meal or snack with carbs before or while drinking. Don’t drink on an empty stomach. Not even one glass.
- Choose low-sugar drinks. Avoid sugary cocktails, sweet wines, and regular soda mixers. Stick to light beer, dry wine, or spirits with soda water and lime. A shot of vodka with soda has about 100 calories and zero sugar. A piña colada? Over 300 calories and 30 grams of sugar.
- Limit how much you drink. Stick to one drink per day for women, two for men. That’s it. More than that increases risk fast.
- Check your blood sugar. Test before you drink, during, and for up to 24 hours after. Many people crash 8-12 hours later. Set an alarm.
- Wear medical ID. If you pass out, someone needs to know you have diabetes. A bracelet or necklace can save your life.
- Tell someone. Let a friend or family member know you have diabetes. Teach them the signs of low blood sugar. Don’t assume they’ll know the difference between drunk and hypoglycemic.

What Your Doctor Should Tell You
A 2021 study found that only 43% of primary care doctors routinely ask diabetic patients about alcohol use. That’s a huge gap. You shouldn’t have to bring it up first.Your doctor should know your meds, your liver function, your history of low blood sugar, and whether you’ve ever had a scary episode after drinking. If they don’t ask, ask them. Say: “I drink occasionally. Is it safe with my meds?”
Diabetes educators now include alcohol in 89% of patient education programs. That’s progress. But if your doctor skips it, you’re left guessing. Don’t guess. Get clear answers.
What’s New in Monitoring
Continuous glucose monitors (CGMs) like the Dexcom G7 and FreeStyle Libre 3 don’t detect alcohol. But they show patterns. If you see your blood sugar drop hours after drinking-even if you didn’t eat-you’ll start to recognize your personal trigger.Some research centers are testing algorithms that predict alcohol-related hypoglycemia based on your meds, activity, and past readings. These tools aren’t available yet, but they’re coming. In the meantime, your CGM is your best early warning system.
The American Diabetes Association updated its guidelines in 2023 to stress individualized risk. There’s no one-size-fits-all rule. Your risk depends on your body, your meds, your liver, and your habits. Only you and your doctor can figure out what’s safe for you.
Final Reality Check
Alcohol doesn’t care about your diabetes. It doesn’t care about your meds. It just wants to be processed. And your liver? It’s already working overtime to keep your blood sugar stable. Adding alcohol is like asking a tired worker to run a marathon.Some people say a glass of red wine is heart-healthy. Maybe. But for someone on insulin or metformin, the risks outweigh the benefits. The liver doesn’t get a day off. Neither does your pancreas. And your brain? It needs steady fuel. Alcohol steals it.
If you’ve ever had a scary low after drinking, you already know the truth. No amount of wine is worth waking up confused, shaking, or in the ER. If you’re unsure, skip it. Your body will thank you.

vinoth kumar
December 2, 2025 AT 04:09Had a friend pass out after a BBQ last summer-thought he was just wasted. Turned out he was hypoglycemic and had insulin on board. Took him 45 minutes to stabilize after glucagon. Never drink on an empty stomach again. Ever.
shalini vaishnav
December 3, 2025 AT 09:05People in the West treat alcohol like it's a wellness trend. In India, we know better-alcohol is a poison disguised as culture. Your liver doesn't care if it's organic wine or cheap whiskey. It just dies slower or faster. Stop romanticizing it.
bobby chandra
December 3, 2025 AT 14:44Let me paint you a picture: your liver is a 3 a.m. shift worker juggling three jobs-detoxing alcohol, regulating glucose, and metabolizing metformin. Now imagine someone hands it a chainsaw and says, ‘Hey, can you fix this too?’ No. Just no. This isn’t a lifestyle choice-it’s a biochemical hostage situation.
Archie singh
December 3, 2025 AT 17:05Of course the ADA says ‘individualized risk’-because they’re too cowardly to say ‘just don’t drink.’ Same people who told us saturated fat was fine until it wasn’t. Your doctor didn’t warn you because they’re paid by pharma to keep you on meds, not to tell you to quit wine.
Gene Linetsky
December 3, 2025 AT 22:04Did you know Big Pharma secretly funds wine companies? That’s why the ‘moderate drinking’ myth persists. The same labs that make metformin also own vineyards. They need you to keep drinking so you keep buying glucose gel and glucagon pens. Wake up. The system is rigged.
Ignacio Pacheco
December 5, 2025 AT 06:41So let me get this straight-you’re telling me I can drink a dry martini with a cheese plate and not crash… but if I have two sips of beer after sushi, I’m a walking medical emergency? Sounds like a glorified game of Russian roulette with carbs.
Jim Schultz
December 5, 2025 AT 17:28YOU NEED TO WEAR A MEDICAL ID!!! Seriously, if you don’t, you’re not just risking your life-you’re risking someone else’s ability to save you!!! Your friend thinks you’re drunk? Then they let you sleep it off? And you die? That’s not tragedy-that’s negligence!!!
Kidar Saleh
December 6, 2025 AT 03:36When I was in London, my diabetic cousin told me he’d never drink again after nearly losing his foot to a nighttime crash. He now carries glucose tabs in his wallet, his coat, his shoes-even his dog’s collar. I thought it was excessive. Now I get it. It’s not about discipline. It’s about survival. And that’s not dramatic. That’s British pragmatism.