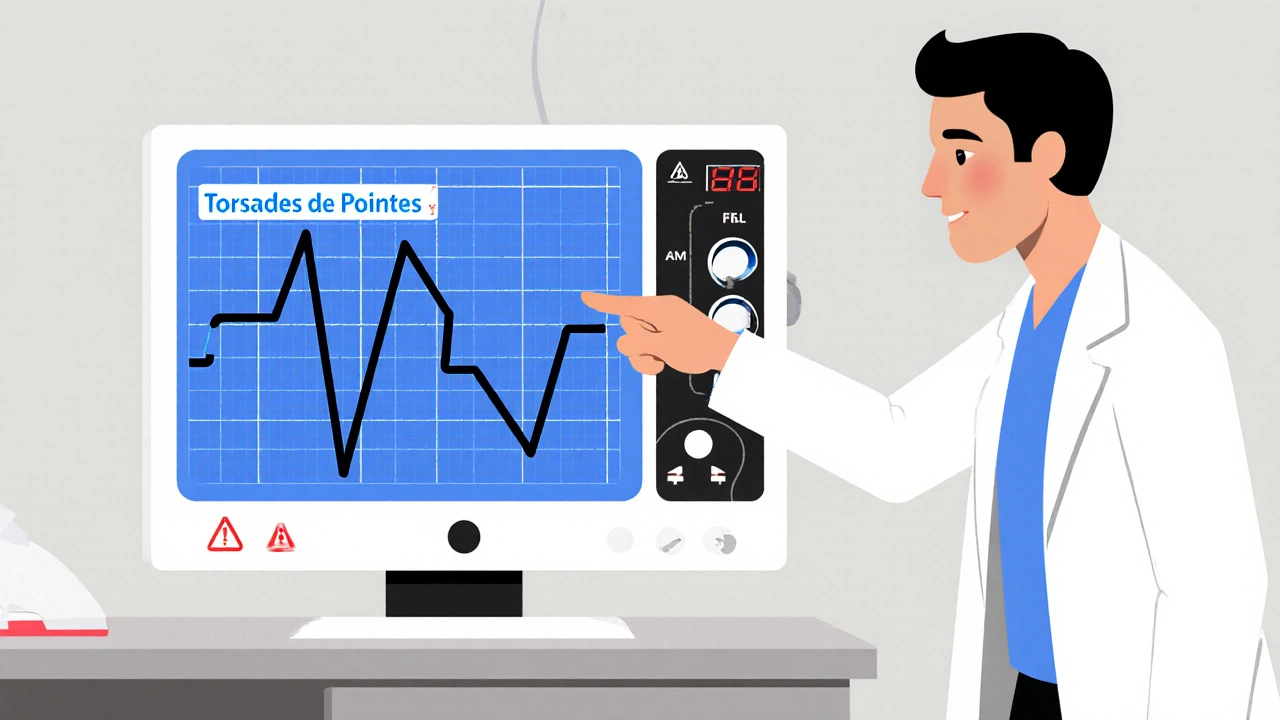
Torsades de Pointes: Causes, Risks, and Medications That Trigger It
When your heart’s electrical system gets disrupted, it can start beating in a wild, chaotic pattern called Torsades de Pointes, a specific type of life-threatening ventricular arrhythmia often linked to prolonged QT intervals on an ECG. Also known as polymorphic ventricular tachycardia, this condition doesn’t just cause dizziness—it can lead to fainting, seizures, or sudden cardiac arrest if not treated fast.
Torsades de Pointes doesn’t happen out of nowhere. It’s usually triggered by something you’re already taking. Many common drugs—like certain antibiotics, antipsychotics, antidepressants, and even some heart meds—can stretch out the QT interval on your ECG. That’s the time your heart takes to recharge between beats. When it gets too long, your heart’s rhythm can spiral out of control. It’s not just about the drug itself, though. Low potassium, low magnesium, or being female can make you way more vulnerable. One study from the Journal of the American College of Cardiology found that over 70% of cases were tied to medications known to prolong the QT interval.
Some of the most common culprits include quinidine, an older antiarrhythmic drug that’s still used in rare cases but carries high torsades risk, sotalol, a beta-blocker with built-in QT-prolonging effects, and erythromycin, a widely prescribed antibiotic that can interfere with heart rhythm. Even some antidepressants, like citalopram and escitalopram, have black box warnings for this exact reason. It’s not just about taking one of these drugs—it’s about stacking them, or having kidney issues, or being dehydrated. That’s when the risk spikes.
What makes Torsades de Pointes tricky is that you might not feel anything until it’s too late. Some people get a flutter in their chest. Others just feel lightheaded. A lot of cases are caught during routine ECGs, especially when someone’s started a new medication. That’s why doctors check your electrolytes and your ECG before and after starting certain drugs. If you’re on any of these meds and suddenly feel faint, dizzy, or like your heart’s skipping beats, don’t wait. Get checked.
There’s no magic cure, but stopping the trigger drug and correcting electrolytes—especially magnesium—can reverse it fast. In severe cases, doctors use pacing or defibrillation. Prevention is the real win. Knowing which drugs to avoid, understanding your own risk factors, and asking your pharmacist or doctor about QT prolongation before starting anything new can save your life.
Below, you’ll find real-world guides on medications that affect heart rhythm, how drug interactions can push you into danger, and what to watch for when you’re on multiple prescriptions. These aren’t theoretical—they’re based on actual cases and clinical advice from people who’ve been there.
Torsades de Pointes from QT‑Prolonging Drugs: How to Spot and Stop It
- Oct, 26 2025
- 11
Learn how to recognise Torsades de Pointes caused by QT‑prolonging drugs, assess risk factors, and apply practical steps to prevent this deadly arrhythmia.
Categories
- Health and Medicine (65)
- Health and Wellness (57)
- Medicine (37)
- Women's Health (11)
- Mental Health (10)
- Men's Health (7)
- Beauty and Wellness (4)
- Health Information (4)
Archives
- March 2026 (1)
- February 2026 (11)
- January 2026 (25)
- December 2025 (28)
- November 2025 (25)
- October 2025 (27)
- September 2025 (14)
- August 2025 (3)
- July 2025 (2)
- June 2025 (2)
- May 2025 (3)
- April 2025 (4)
- online pharmacy
- medication safety
- dietary supplement
- health benefits
- dietary supplements
- generic drugs
- prevention
- fertility
- online pharmacy Australia
- side effects
- QT prolongation
- medication side effects
- diabetes medications
- GLP-1 agonists
- nocebo effect
- brand vs generic
- treatment
- treatment options
- benefits
- connection
