Torsades de Pointes from QT‑Prolonging Drugs: How to Spot and Stop It
 Oct, 26 2025
Oct, 26 2025
QTc Interval Calculator
Calculated QTc Interval:
• Normal QTc: < 450ms (men), < 460ms (women)
• High risk: QTc ≥ 500ms
• Always consider electrolyte levels and other risk factors
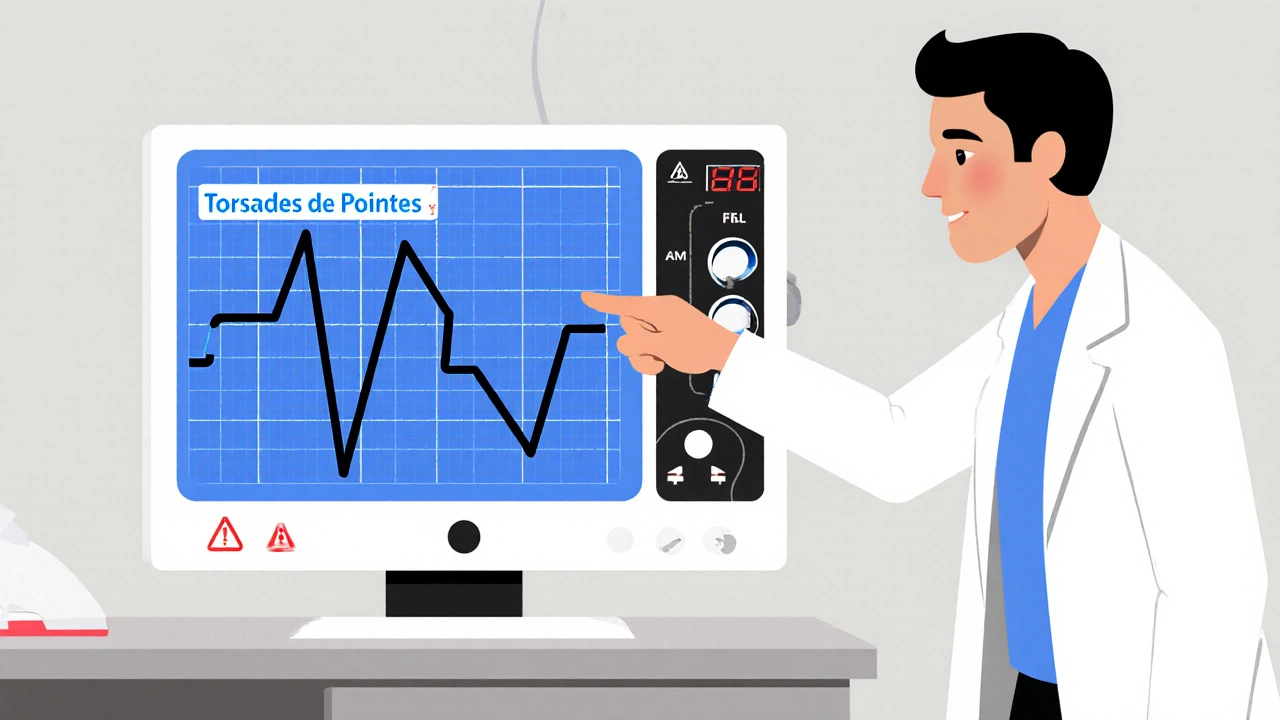
When a patient’s heart rhythm suddenly twists into an erratic, sine‑wave pattern on the monitor, the culprit is often Torsades de Pointes a rare but life‑threatening form of polymorphic ventricular tachycardia that only appears when the QT interval is prolonged. If you’ve ever wondered why a simple antibiotic or an anti‑psychotic can turn a heartbeat into a ticking time bomb, this guide will walk you through the science, the red‑flag signs, and the concrete steps you can take to keep patients safe.
Why the QT Interval Matters
The QT interval the time from the start of the Q wave to the end of the T wave on an ECG, reflecting ventricular repolarisation should stay under roughly 450 ms in men and 460 ms in women. When drugs interfere with the heart’s potassium channels-especially the hERG channel a protein that conducts the rapid delayed rectifier potassium current (I_Kr) essential for phase‑3 of the cardiac action potential-the QT stretches, early after‑depolarizations appear, and TdP can erupt.
Who’s at Risk? The Numbers Talk
In the general population, drug‑induced QT prolongation leads to about 2.5 cases per million men and 4.0 per million women each year. Women, older adults, and patients with electrolyte disturbances (low potassium or magnesium) bear the bulk of the risk. For example, serum potassium < 3.5 mmol/L triples the chance of TdP, while magnesium < 1.6 mg/dL nearly triples it again. Add bradycardia (< 60 bpm) or a pre‑existing heart condition, and the odds climb sharply.
High‑Risk Medications Worth Memorising
More than 200 drugs sit on the “QT‑prolonging” list, but a handful pop up in everyday practice. Below is a quick look‑up table that breaks them into the three CredibleMeds risk tiers.
| Medication | Risk Tier | Typical Dose Limit | Monitoring Recommendation |
|---|---|---|---|
| Methadone | Known | ≤ 100 mg/day (higher doses increase risk) | Baseline ECG, repeat at 1 week and after each 25 mg increase |
| Ondansetron (IV) | Known | ≤ 16 mg IV | ECG if dose > 8 mg or patient has other risk factors |
| Citalopram | Known | ≤ 40 mg/day (≤ 20 mg/day in > 65 yr) | ECG after dose escalation, check electrolytes |
| Haloperidol | Possible | ≤ 5 mg IV bolus | ECG if cumulative dose > 20 mg or IV use |
| Erythromycin | Conditional | Standard dosing | ECG when combined with other QT‑prolongers or if electrolytes abnormal |
Remember, the “Known” tier means solid evidence of TdP; “Possible” is less certain, and “Conditional” only becomes dangerous when other factors stack up.
The 5‑Step Prevention Checklist
What can you do before you write a prescription? Here’s a practical, step‑by‑step cheat sheet that fits into any clinic workflow.
- Screen for congenital long QT syndrome. Use the Schwartz score (≥ 3 points = high probability) if there’s a family history of sudden cardiac death.
- Audit electrolytes. Aim for potassium ≥ 4.0 mmol/L and magnesium ≥ 2.0 mg/dL. Replace before starting the drug.
- Check the medication list. Run every prescription through CredibleMeds the online database that categorises drugs by TdP risk and flag any known or conditional agents.
- Obtain a baseline ECG. Measure QTc using Bazett’s formula; if QTc ≥ 500 ms, look for alternatives.
- Plan ongoing monitoring. Repeat ECG after dose changes, after adding a second QT‑prolonger, or if the patient develops bradycardia.
If any step raises a red flag, either choose a safer drug or set up tighter surveillance.
What to Do When TdP Strikes
Time is muscle-literally. The first minutes decide whether the episode stops on its own or spirals into ventricular fibrillation.
- IV magnesium sulfate. Give 1‑2 g over 5-10 minutes. It works in about 80 % of cases, even if serum magnesium is already normal.
- Increase heart rate. Temporary pacing to keep HR > 90 bpm or isoproterenol infusion can suppress early after‑depolarizations.
- Remove the offending drug. Stop the QT‑prolonger immediately and consider a lipid emulsion if the drug is highly lipophilic (e.g., certain anti‑arrhythmics).
- Correct electrolytes. Push potassium to > 4.5 mmol/L and magnesium to > 2.2 mg/dL.
Call the code team, attach a defibrillator, and be ready to shock if the rhythm degenerates.

Emerging Tools That Make Prevention Easier
Artificial‑intelligence models from Mayo Clinic now combine 17 clinical variables (age, sex, QTc, electrolytes, renal function, etc.) to predict individual TdP risk with 89 % accuracy. Many hospitals are integrating these scores into their electronic medical records, flagging high‑risk patients before a prescription is even written.
On the regulatory side, the FDA’s 2023 draft guidance on QT/QTc modelling lets sponsors replace the classic “thorough QT” study with concentration‑QT models, shortening drug development timelines while still protecting patients.
Key Takeaways
- QT‑prolongation is the gateway to Torsades de Pointes; keep QTc < 500 ms whenever possible.
- Electrolyte correction, baseline ECG, and medication review cut the risk dramatically.
- High‑risk drugs (methadone, ondansetron IV, citalopram) need strict dosing limits and repeat ECGs.
- Acute TdP is treated first with magnesium, then heart‑rate acceleration and drug cessation.
- AI risk scores and newer QT modelling are making personalized prevention a reality.
What QTc value should trigger a medication change?
Guidelines advise stopping or substituting the drug when QTc reaches 500 ms or shows an increase of 60 ms from baseline.
Can a patient with normal electrolytes still develop TdP?
Yes. Factors like genetic hERG variants, bradycardia, or simultaneous use of multiple QT‑prolongers can provoke TdP even when electrolytes are within range.
How often should I repeat an ECG after starting a high‑risk drug?
A baseline ECG is mandatory. Then repeat at 1 week, after any dose increase, and whenever the patient develops symptoms like dizziness or palpitations.
Is magnesium therapy safe for all patients?
Generally yes; the dose used for TdP (1‑2 g IV) rarely causes hypermagnesemia. Watch for renal failure patients and monitor serum levels if large repeat doses are needed.
What role does the hERG channel play in drug safety testing?
All new drugs must be screened for hERG blockade because inhibition directly lengthens the QT interval. A positive hERG result usually triggers additional in‑vivo QT studies or concentration‑QT modeling.

Brady Johnson
October 26, 2025 AT 11:32Whoa, this post reads like a textbook tax audit on every QT‑prolonger out there-dramatic, exhaustive, and somehow still missing the point that most clinicians just need a quick cheat sheet, not a PhD dissertation. The tables are nice, but the endless warnings feel like a guilt‑trip for anyone daring to prescribe opioids or anti‑nausea meds. You’re basically saying “don’t prescribe anything” while pretending to empower us. If you wanted to save lives, a one‑page flowchart would have done the trick. Still, kudos for the thoroughness, even if it’s a bit over the top.
Jay Campbell
October 27, 2025 AT 15:23Good point, thanks for the summary.
Laura Hibbard
October 28, 2025 AT 19:26Oh wow, another epic saga on QT prolongation that makes me wish I’d paid more attention in med school. Because nothing screams excitement like a five‑point checklist that reads like a corporate onboarding form. I love how the article reminds us that a potassium level of 4.0 is the holy grail, as if we’ve been living in a desert of electrolytes. And the mention of AI risk scores? Great, now my ECG machine will judge me more harshly than my mother. The list of ‘high‑risk’ meds reads like a grocery list for a pharmacy that’s lost its mind. Seriously, methadone, ondansetron, citalopram-who knew these everyday heroes could double as heart‑killers? The five‑step prevention checklist is basically a survival guide for a post‑apocalyptic clinic. Step one: screen for congenital Long QT-because who doesn’t have a secret family history of sudden cardiac death? Step two: audit electrolytes-yes, let’s chase every millimole like we’re plating medals. Step three: check the med list-maybe we should also check the garbage list while we’re at it. Step four: baseline ECG-nothing like a quick snapshot of a heart that might explode later. Step five: ongoing monitoring-because why stop when you can keep watching the clock tick. When TdP actually strikes, the article’s heroics of magnesium and pacing feel like a superhero landing in the ER. I can already picture the code team shouting, ‘Give me the magnesium!’ like it’s a magic spell. All in all, this guide is the ultimate mixtape of cautionary tales, tech jargon, and semi‑dramatic flair that will keep us up at night-cheers!
Lori Brown
October 29, 2025 AT 23:30Absolutely love the upbeat tone here 😊! The checklist is super handy and the AI tools sound promising. Keep sharing these gems!
Rhea Lesandra
October 31, 2025 AT 03:33Great reminder to check electrolytes before starting QT‑prolongers. It's amazing how a simple step like ensuring potassium is above 4.0 mmol/L can act as a silent guardian, preventing the cascade of electrical instability that could otherwise culminate in a terrifying bout of torsades, especially when patients are already juggling multiple comorbidities and polypharmacy that each adds a layer of risk. Also, the baseline ECG recommendation is spot on. By integrating these straightforward actions into routine practice, we create a safety net that catches potential arrhythmias before they become catastrophic, ultimately improving patient outcomes and reducing the panic that can arise when a monitor suddenly spikes into a sine‑wave pattern.
Kasey Marshall
November 1, 2025 AT 07:36Check meds run credibled meds database get baseline ecg see electrolytes correct if needed repeat ecg after dose changes
Dave Sykes
November 2, 2025 AT 11:40Here’s the thing: you don’t need to be a cardiology wizard to apply this. Start with a quick med review, grab that baseline QTc, and if it’s creeping toward 500 ms, swap the drug now. Keep the potassium and magnesium in the safe zone and you’ll cut the risk dramatically. This approach is practical and saves lives-no excuses.
Erin Leach
November 3, 2025 AT 15:43I hear you, the constant vigilance can feel overwhelming, but having a simple checklist really helps keep everything straight. When you see a patient’s QTc edging up, a quick electrolyte boost and a call to the pharmacist can make all the difference. You’ve got this.
Erik Redli
November 4, 2025 AT 19:46Honestly, this whole “avoid any QT‑prolonger” mindset is overblown; clinicians can handle these meds with proper monitoring. Turning every prescription into a red‑flag parade just creates unnecessary fear.
Tim Waghorn
November 5, 2025 AT 23:50While I acknowledge the concerns raised, it is essential to recognize that the evidence supporting routine cessation of all QT‑prolonging agents in the absence of a QTc exceeding 500 ms remains inconclusive. A balanced approach, incorporating risk stratification tools and adhering to established dosing guidelines, is advisable.
Paul Luxford
November 7, 2025 AT 03:53Thanks for the thorough overview; the emphasis on baseline ECG and electrolyte management aligns well with current practice standards.