QT Prolongation: What It Is, Which Drugs Cause It, and How to Stay Safe
When your heart’s electrical system gets thrown off, it can lead to something called QT prolongation, a delay in the heart’s electrical recovery phase that can trigger dangerous irregular heartbeats. Also known as long QT syndrome, it’s not always genetic—often, it’s caused by everyday medications you might be taking. This isn’t just a lab finding. Left unchecked, it can lead to a life-threatening rhythm called torsades de pointes, where your heart quivers instead of pumping blood properly.
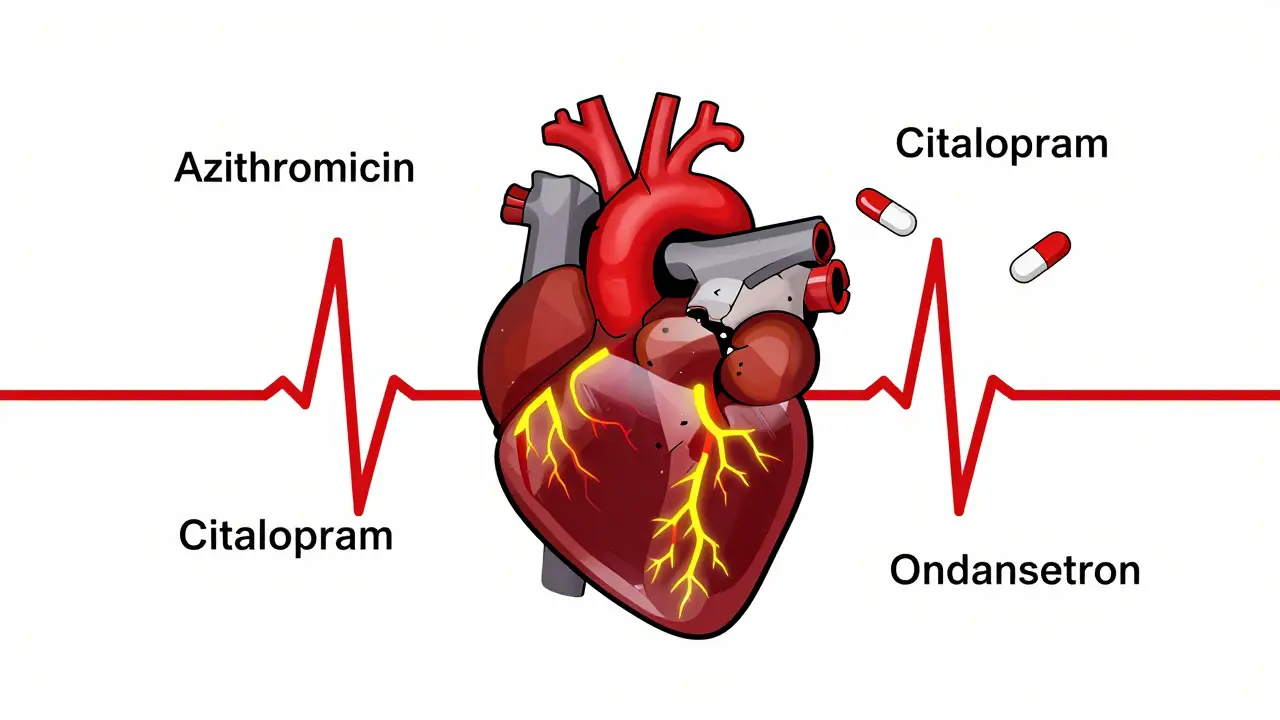
Many common drugs can mess with your heart’s timing. Antidepressants like citalopram and escitalopram, certain antibiotics like azithromycin, and even some anti-nausea pills like ondansetron are known to stretch out the QT interval. Even something as simple as caffeine can add up when combined with other meds, especially if you’re on warfarin or thyroid meds. It’s not about avoiding all meds—it’s about knowing which ones carry this risk and how to manage them. People on multiple prescriptions are at higher risk, especially older adults or those with existing heart conditions.
It’s not just the drug itself—it’s the combo. A pill that’s fine alone might become risky when stacked with another that also affects QT. For example, taking an antifungal like fluconazole with an antidepressant like sertraline? That’s a red flag. Doctors check your electrolytes, your kidney function, and your full med list before prescribing. But if you’re managing your own meds, you need to ask: Could this be affecting my heart? Symptoms like dizziness, fainting, or a racing heartbeat aren’t normal. They’re warnings.
Some of the posts here dig into how medications interact in ways you wouldn’t expect. You’ll find guides on antidepressants that cause weight gain—many of those same drugs also affect heart rhythm. Others cover how caffeine can interfere with blood thinners, and how even common pain relievers like diclofenac gel can carry hidden risks when used long-term. There’s also deep dives into diabetes drugs, ED meds, and diuretics—all of which can influence your heart’s electrical activity in subtle ways.
You don’t need to panic. But you do need to be aware. If you’re on any of these meds, talk to your doctor about getting a simple ECG. It’s quick, painless, and can catch a problem before it becomes serious. This page pulls together real-world examples from actual medication guides so you can spot the patterns, ask the right questions, and stay in control of your health—one pill at a time.
Heart Arrhythmias from Medications: Warning Signs and What to Do
- Jan, 18 2026
- 9
Many common medications can trigger dangerous heart rhythm problems. Learn the warning signs like palpitations, dizziness, and fainting, and what to do if you suspect a drug is affecting your heart. Preventable and treatable.
ECG Monitoring During Macrolide Therapy: Who Really Needs It?
- Dec, 1 2025
- 9
Macrolide antibiotics like azithromycin can cause dangerous heart rhythm changes. Learn who needs an ECG before taking them-and why skipping this step can be risky.
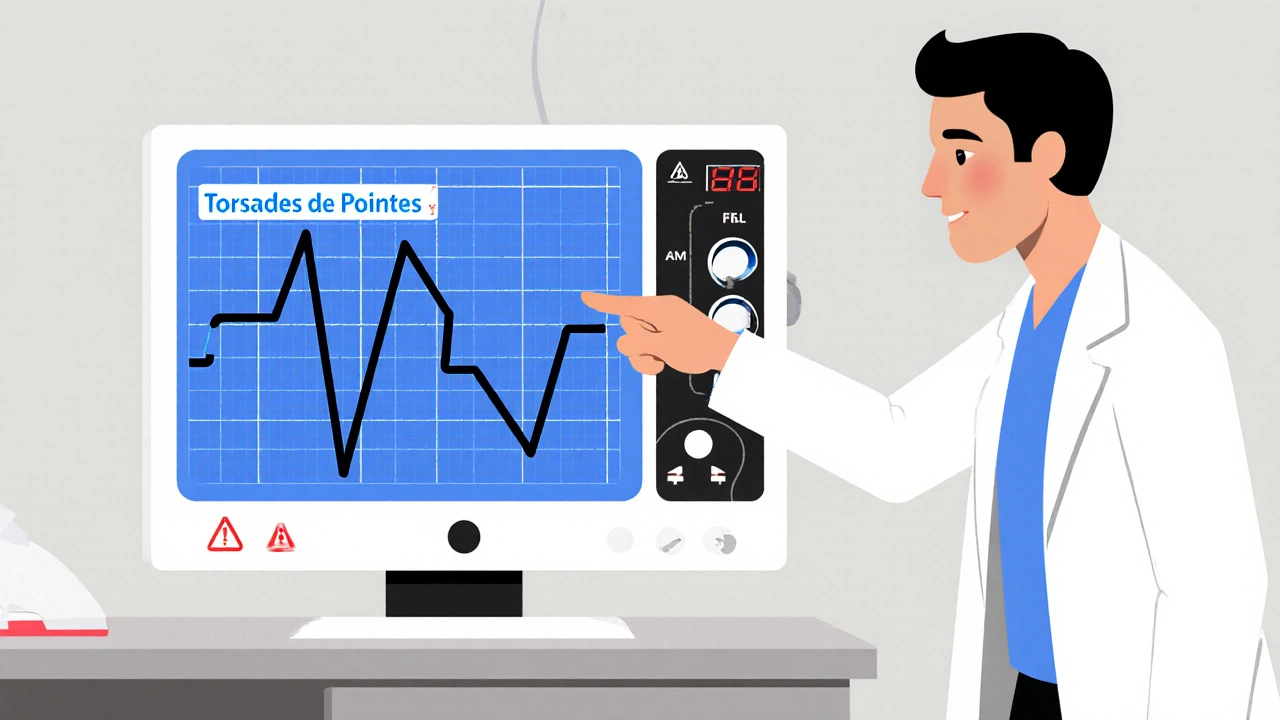
Torsades de Pointes from QT‑Prolonging Drugs: How to Spot and Stop It
- Oct, 26 2025
- 11
Learn how to recognise Torsades de Pointes caused by QT‑prolonging drugs, assess risk factors, and apply practical steps to prevent this deadly arrhythmia.
Categories
- Health and Medicine (65)
- Health and Wellness (57)
- Medicine (37)
- Women's Health (11)
- Mental Health (10)
- Men's Health (7)
- Beauty and Wellness (4)
- Health Information (4)
Archives
- March 2026 (1)
- February 2026 (11)
- January 2026 (25)
- December 2025 (28)
- November 2025 (25)
- October 2025 (27)
- September 2025 (14)
- August 2025 (3)
- July 2025 (2)
- June 2025 (2)
- May 2025 (3)
- April 2025 (4)
- online pharmacy
- medication safety
- dietary supplement
- health benefits
- dietary supplements
- generic drugs
- prevention
- fertility
- online pharmacy Australia
- side effects
- QT prolongation
- medication side effects
- diabetes medications
- GLP-1 agonists
- nocebo effect
- brand vs generic
- treatment
- treatment options
- benefits
- connection
