Metformin and Alcohol: What You Need to Know Before You Drink
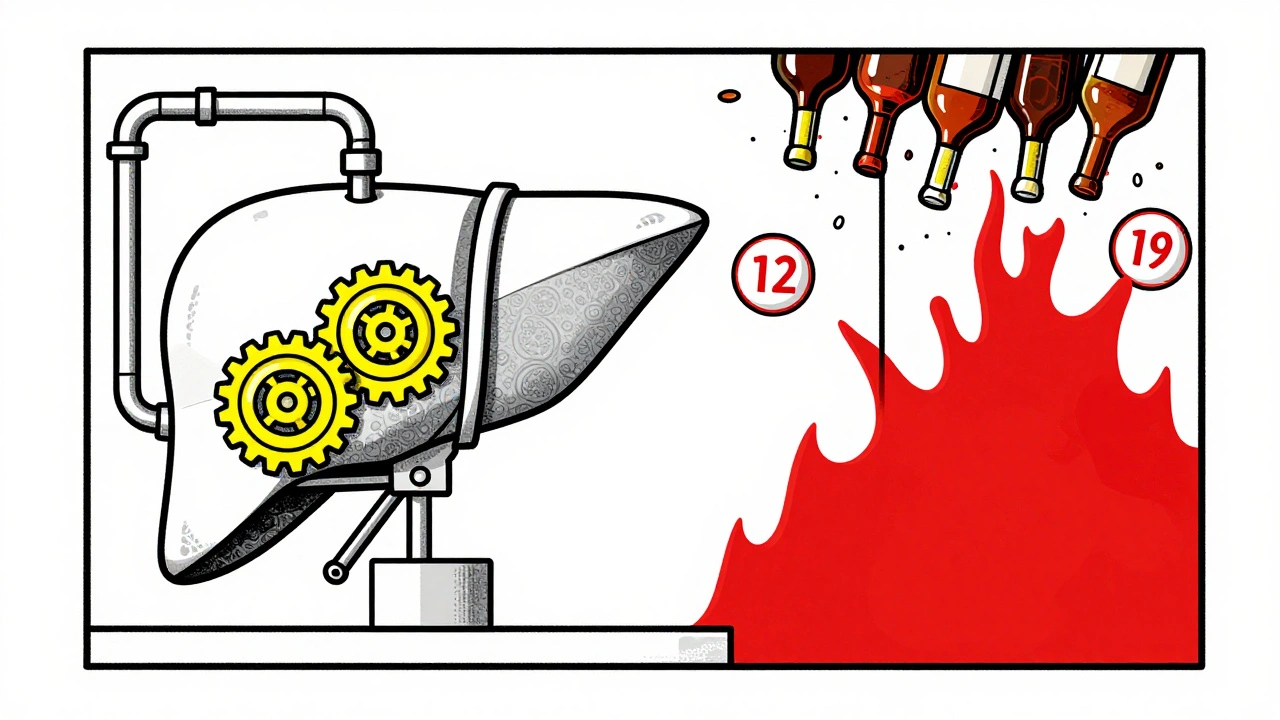
When you take metformin, a first-line medication for type 2 diabetes that helps lower blood sugar by reducing liver glucose production and improving insulin sensitivity. It's one of the most prescribed drugs in the world, trusted for its effectiveness and low cost. But if you drink alcohol, even occasionally, you’re playing with fire. Not because it cancels out the drug—but because together, they can trigger something dangerous: lactic acidosis, a rare but life-threatening buildup of lactic acid in the blood, often linked to metformin use when combined with alcohol or kidney issues.
Here’s the real issue: alcohol slows down how your liver processes lactate. Metformin already makes your body produce a bit more of it. Put them together, and your body can’t keep up. The result? A dangerous chemical imbalance. This isn’t theoretical—it’s been documented in emergency rooms. People who drink while on metformin, especially if they’re older, have kidney problems, or drink heavily, are at higher risk. Even one or two drinks can be enough to tip the scale if your system is already under stress.
It’s not just about lactic acidosis, either. Alcohol lowers blood sugar on its own. So if you’re taking metformin—already working to bring your glucose down—you could end up with a crash. Symptoms like dizziness, sweating, confusion, or a rapid heartbeat might be written off as "just a hangover," but they could be signs of severe hypoglycemia. And if you’re drinking on an empty stomach or skipping meals? The risk spikes.
Some people think, "I’m only having a beer on weekends," or "I drink wine with dinner." But it’s not about how much—it’s about how often and how your body reacts. If you’ve had kidney trouble, liver disease, or heart failure, your doctor likely already told you to avoid alcohol. If not, ask. There’s no official "safe" amount, but most guidelines say: if you drink, do it rarely, never on an empty stomach, and always monitor your blood sugar.
And here’s what most people miss: diabetes medication safety, the broader practice of understanding how drugs interact with food, alcohol, and other meds to prevent harm isn’t just about taking pills on time. It’s about knowing what your body can handle. That’s why posts like "Choosing Diabetes Medications Based on Side Effect Profiles" and "Diabetes Medications for Seniors" exist—they show you that every pill has a context. Metformin works great for many, but it’s not magic. It needs smart habits to stay safe.
You don’t have to quit alcohol forever. But you do need to treat it like a variable in your diabetes equation—something that changes the outcome. Talk to your doctor. Get your kidney function checked. Learn the early warning signs of lactic acidosis: muscle pain, trouble breathing, unusual tiredness, stomach upset. If you feel these after drinking, don’t wait—get help.
Below, you’ll find real, practical advice from people who’ve been there—how to spot the hidden risks, what doctors actually recommend, and how to manage your health without feeling like you’re giving up everything. This isn’t about fear. It’s about control.
Alcohol and Diabetes Medications: How Drinking Affects Blood Sugar and Liver Health
- Dec, 1 2025
- 8
Drinking alcohol while on diabetes meds can cause dangerous drops in blood sugar and harm your liver. Learn how metformin, insulin, and sulfonylureas interact with alcohol-and what you can do to stay safe.
Categories
- Health and Medicine (63)
- Health and Wellness (57)
- Medicine (37)
- Women's Health (11)
- Mental Health (9)
- Men's Health (7)
- Beauty and Wellness (4)
- Health Information (4)
Archives
- February 2026 (9)
- January 2026 (25)
- December 2025 (28)
- November 2025 (25)
- October 2025 (27)
- September 2025 (14)
- August 2025 (3)
- July 2025 (2)
- June 2025 (2)
- May 2025 (3)
- April 2025 (4)
- March 2025 (4)
- online pharmacy
- medication safety
- dietary supplement
- health benefits
- dietary supplements
- generic drugs
- prevention
- fertility
- online pharmacy Australia
- side effects
- QT prolongation
- medication side effects
- diabetes medications
- GLP-1 agonists
- nocebo effect
- brand vs generic
- treatment
- treatment options
- benefits
- connection
