Biosimilars: What They Are, How They Work, and Why They Matter
When you hear biosimilars, highly similar versions of complex biologic drugs made after the original patent expires. Also known as follow-on biologics, they work just like the original but cost far less—often 15% to 30% cheaper. Unlike regular generic pills, which are simple chemical copies, biosimilars are made from living cells, so they’re not exact duplicates. But they’re close enough that the FDA and other global regulators say they’re just as safe and effective.
They’re not just about saving money. Biosimilars help patients who can’t afford expensive biologics for conditions like rheumatoid arthritis, Crohn’s disease, or certain cancers. For example, a biosimilar to Humira can cut monthly costs from over $2,000 to under $1,000. That’s life-changing for people on fixed incomes or without good insurance. And because they’re based on real-world data from the original drug, doctors know what to expect—side effects, dosing, how they interact with other meds.
But there’s confusion. Some patients think biosimilars are like over-the-counter painkillers—just a cheaper version of the same thing. They’re not. They’re more like a slightly different recipe for the same cake: same taste, same texture, same effect, but made with a different oven. That’s why switching from a brand-name biologic to a biosimilar needs to be done carefully, under a doctor’s watch. Pharmacists can’t swap them automatically like they can with aspirin or metformin. In fact, state laws on substitution vary, and some require the prescriber to approve the switch.
That’s where things get tricky. If you’re on a biologic for an autoimmune disease, your body might respond differently to a biosimilar—even if it’s approved as equivalent. That’s why studies track real-world outcomes: how many people stay on the drug, how often they need to switch back, and whether flare-ups increase. The good news? Most patients do just fine. The bad news? Some providers still hesitate, not because the science is weak, but because they’re used to the original brand.
And it’s not just about the drug itself. Biosimilars change how pharmacies, insurers, and hospitals manage inventory. They force conversations about cost versus comfort. They push pharmacists to explain the difference between a generic pill and a biosimilar injection. They make patients ask: Is this really the same? And the answer, backed by years of data and millions of doses given, is usually yes.
You’ll find posts here that dig into real cases: how biosimilars interact with antacids and antibiotics, how they’re used in elderly patients, and how they fit into broader medication safety plans. Some posts show how switching to a biosimilar can reduce hospital visits. Others warn about rare side effects that might pop up only after months on the new drug. There’s no hype here—just facts, patient stories, and practical advice from people who’ve been there.
Future of Global Generic Markets: Key Trends and Predictions for 2025-2030
- Jan, 21 2026
- 8
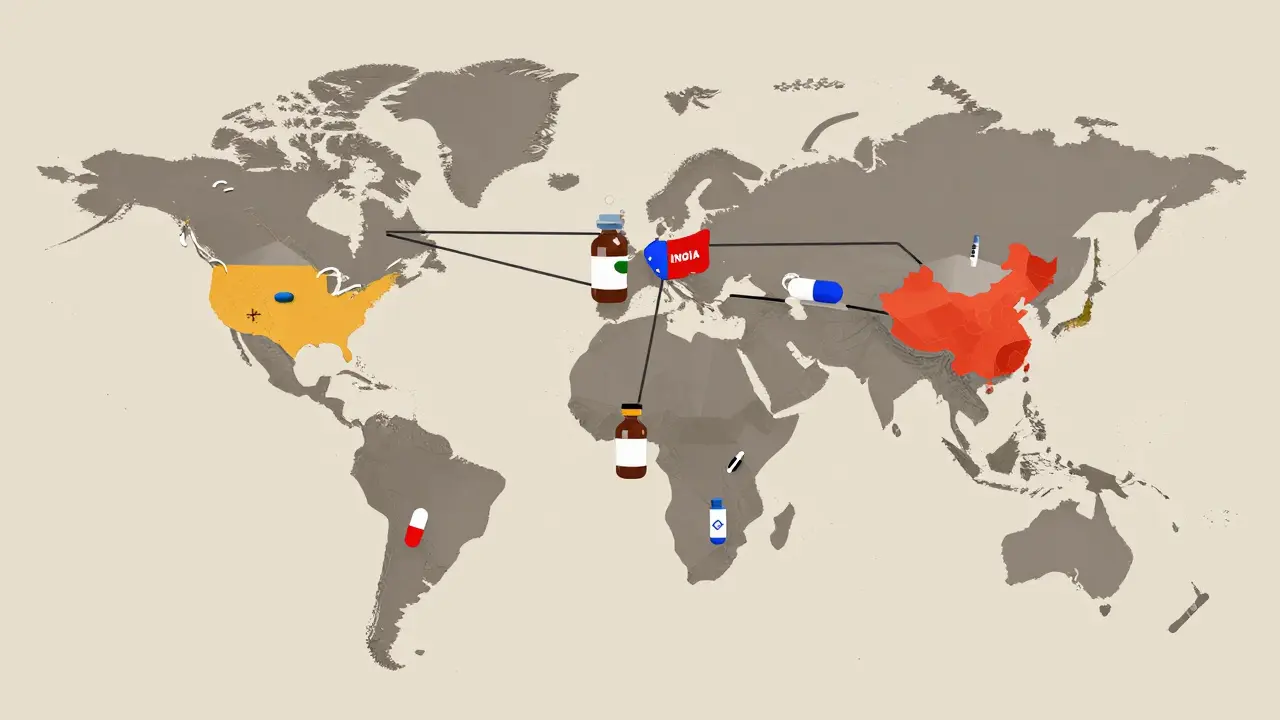
The global generic drug market is growing fast, driven by rising chronic diseases and cost pressures. India and China lead manufacturing, while biosimilars and emerging markets shape the future. Generics remain essential for affordable care worldwide.

Clinical Outcomes with Biosimilars: Do They Work as Well as the Original Biologics?
- Nov, 24 2025
- 14
Biosimilars are proven to work as well as original biologic drugs in treating cancer, autoimmune diseases, and more. They're safer, cheaper, and backed by over a decade of global clinical data.
Categories
- Health and Medicine (62)
- Health and Wellness (57)
- Medicine (37)
- Women's Health (11)
- Mental Health (9)
- Men's Health (7)
- Beauty and Wellness (4)
- Health Information (4)
Archives
- February 2026 (8)
- January 2026 (25)
- December 2025 (28)
- November 2025 (25)
- October 2025 (27)
- September 2025 (14)
- August 2025 (3)
- July 2025 (2)
- June 2025 (2)
- May 2025 (3)
- April 2025 (4)
- March 2025 (4)
- online pharmacy
- medication safety
- dietary supplement
- health benefits
- dietary supplements
- generic drugs
- prevention
- fertility
- online pharmacy Australia
- side effects
- QT prolongation
- medication side effects
- diabetes medications
- GLP-1 agonists
- nocebo effect
- brand vs generic
- treatment
- treatment options
- benefits
- connection
