Antibiotic Yeast Infection: What You Need to Know
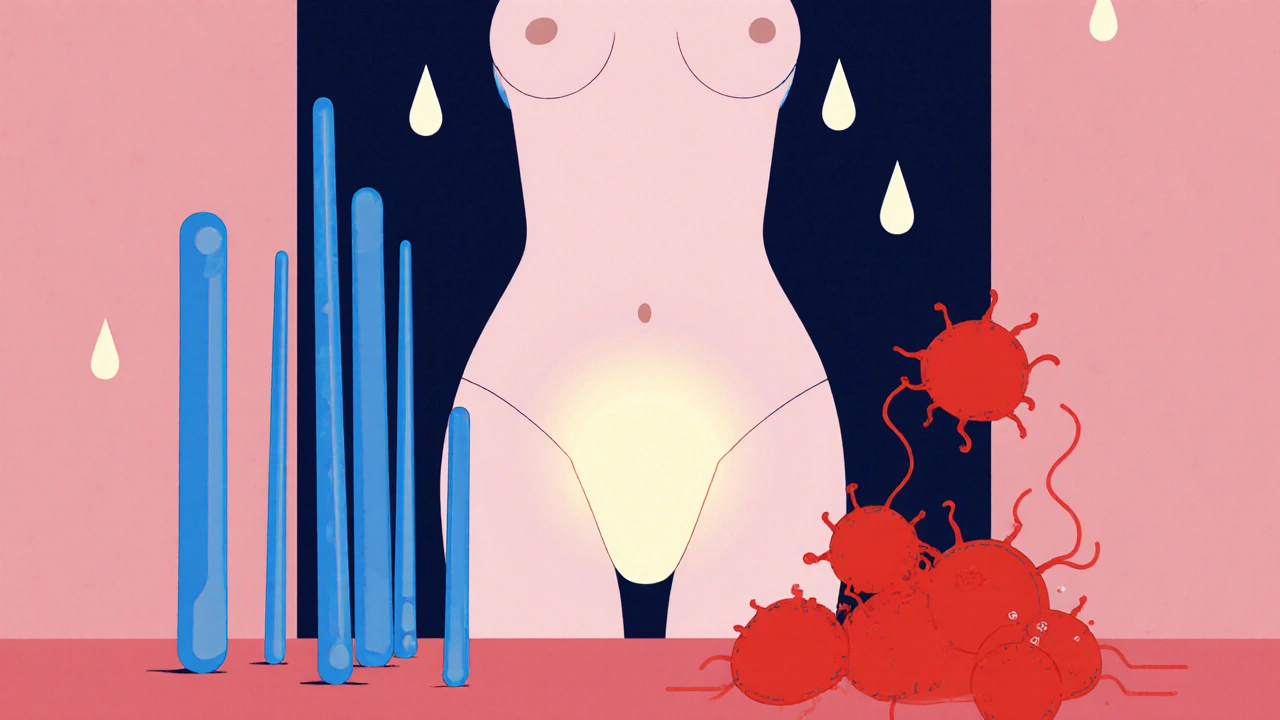
When you take an antibiotic, a medication designed to kill harmful bacteria. Also known as antibacterial drugs, they’re essential for treating infections like pneumonia or strep throat—but they don’t discriminate. They wipe out good bacteria too, especially in your gut and vagina. This disruption can let Candida, a type of fungus that normally lives harmlessly in your body. Also known as yeast, it grow out of control and cause a yeast infection. It’s not rare. About 1 in 3 women will get one after a course of antibiotics, and men can get them too—especially after long-term use.
Not all antibiotics cause this equally. Broad-spectrum ones like amoxicillin, ciprofloxacin, and doxycycline are the usual suspects. They hit a wide range of bacteria, leaving fewer defenders to keep Candida in check. Meanwhile, narrow-spectrum antibiotics like penicillin are less likely to trigger it. The problem isn’t just the drug—it’s how you use it. Taking antibiotics when you don’t need them, skipping doses, or not finishing the full course makes resistance worse and increases your risk of side effects like yeast overgrowth. This isn’t just about discomfort; it’s about balance. Your body’s microbiome is a living ecosystem. When you knock out the good guys, the opportunists move in.
Yeast infections from antibiotics aren’t just a nuisance—they’re a sign your system is out of sync. Symptoms include itching, burning, thick white discharge, and redness. In men, it can mean redness or irritation on the penis. If you’ve been on antibiotics and suddenly feel off down there, it’s not your imagination. Many people reach for over-the-counter antifungals like clotrimazole or fluconazole, and those often work. But the real fix isn’t just killing the yeast—it’s restoring the environment that kept it in check. Probiotics, especially those with Lactobacillus strains, can help. Eating yogurt with live cultures isn’t a cure, but it’s a simple step. Avoid sugar-heavy foods, which feed yeast. And if it keeps coming back? That’s not normal. It could mean an underlying issue like diabetes or a weakened immune system.
You’ll find posts here that dig into how antibiotics interact with other meds—like how antacids can reduce antibiotic effectiveness, or how warfarin and antibiotics can dangerously combine. You’ll also see how mupirocin resistance develops from overuse, and how deprescribing helps older adults avoid unnecessary drug chains. These aren’t random topics. They’re all part of the same story: how drugs affect your body beyond their intended target. Antibiotic yeast infections are a side effect, yes—but they’re also a warning. Your body is trying to tell you something. The posts below give you the facts, not the fluff, so you can protect yourself, your family, and your health—one pill at a time.
Antibiotic-Induced Yeast Infections: How to Prevent and Treat Them
- Nov, 17 2025
- 9
Antibiotic-induced yeast infections are common but preventable. Learn how to stop them before they start with probiotics, antifungals, and lifestyle changes-and what to do if you already have symptoms.
Categories
- Health and Medicine (65)
- Health and Wellness (57)
- Medicine (37)
- Women's Health (11)
- Mental Health (10)
- Men's Health (7)
- Beauty and Wellness (4)
- Health Information (4)
Archives
- March 2026 (1)
- February 2026 (11)
- January 2026 (25)
- December 2025 (28)
- November 2025 (25)
- October 2025 (27)
- September 2025 (14)
- August 2025 (3)
- July 2025 (2)
- June 2025 (2)
- May 2025 (3)
- April 2025 (4)
- online pharmacy
- medication safety
- dietary supplement
- health benefits
- dietary supplements
- generic drugs
- prevention
- fertility
- online pharmacy Australia
- side effects
- QT prolongation
- medication side effects
- diabetes medications
- GLP-1 agonists
- nocebo effect
- brand vs generic
- treatment
- treatment options
- benefits
- connection
