Antibiotic-Induced Yeast Infections: How to Prevent and Treat Them
 Nov, 17 2025
Nov, 17 2025
Antibiotic Yeast Infection Risk Calculator
Calculate Your Risk
Antibiotics disrupt your vaginal flora and can lead to yeast infections. This tool estimates your risk based on your treatment and lifestyle factors.
When you take an antibiotic for a sore throat, a sinus infection, or a urinary tract infection, you’re not just killing the bad bacteria-you’re also wiping out the good ones. And one of the most common side effects? A yeast infection. It’s not rare. In fact, up to 30% of people with vaginas develop one after antibiotics. The itching, burning, and thick white discharge can come out of nowhere, right when you’re trying to feel better. But here’s the thing: you don’t have to just wait it out. There are real, proven ways to prevent it-and treat it fast if it happens.
Why Antibiotics Cause Yeast Infections
Your vagina isn’t a sterile place. It’s home to trillions of bacteria, mostly Lactobacillus, that keep things balanced. These good bugs make lactic acid, which keeps your vaginal pH low-between 3.8 and 4.5. That acidic environment stops yeast like Candida albicans from taking over. But broad-spectrum antibiotics like amoxicillin, tetracycline, or ciprofloxacin don’t discriminate. They kill off Lactobacillus along with the harmful bacteria. Without those protective bugs, yeast grows unchecked. The result? A classic yeast infection.
It’s not just about the antibiotic, though. Other things make it worse. High blood sugar-even from diabetes or medications like Jardiance-feeds yeast. Tight synthetic underwear traps heat and moisture, creating the perfect breeding ground. Douching strips away protective bacteria. And if you’re on birth control pills or pregnant, higher estrogen levels can also tip the scales in yeast’s favor.
What a Yeast Infection Really Feels Like
Most people know the signs: intense itching, burning when you pee or have sex, and a thick, white discharge that looks like cottage cheese. But here’s what most don’t realize: nearly two out of five women who think they have a yeast infection actually have something else-bacterial vaginosis, a UTI, or even a skin condition. That’s why self-diagnosing can backfire. If you use an antifungal cream when you don’t have yeast, you’re wasting time and making the real problem worse.
True yeast infections usually respond quickly to treatment. But if you’ve had four or more in a year, you’re dealing with recurrent candidiasis. That’s not normal. It means something’s out of balance-and antibiotics are often the trigger.
How to Prevent a Yeast Infection While Taking Antibiotics
You don’t have to wait until you’re itching to act. Prevention works better than reaction. Here’s what actually helps, backed by research and clinical experience.
- Start an antifungal at the same time as your antibiotic. Over-the-counter options like clotrimazole (Gyne-Lotrimin) or miconazole (Monistat) are safe and effective. Use the 7-day cream or suppository-not the one-dose version. Studies show the longer course is 15% more effective at stopping yeast before it starts.
- Take a probiotic with the right strains. Not all probiotics are the same. Look for Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14. These strains have been shown to reduce yeast infections by half when taken daily at 10 billion CFUs. Brands like Fem-Dophilus or Culturelle Women’s Healthy Balance contain these. Take them at least two hours before or after your antibiotic so they survive.
- Ditch the sugar and refined carbs. Yeast feeds on glucose. Cutting out white bread, pastries, candy, and sugary drinks can lower your risk. A 2021 review found that even strict low-sugar diets only reduced recurrence by 15-20%, so don’t rely on this alone-but it helps.
- Wear cotton underwear. Synthetic fabrics trap heat and moisture. Cotton keeps things dry and cool. Studies show vaginal temperature drops from 36-38°C in synthetics to 32-34°C in cotton, cutting yeast growth by half.
- Avoid douches, scented tampons, and bubble baths. These disrupt your natural pH. Douching removes 70-90% of your protective bacteria. Your vagina cleans itself. You don’t need to help.
The most successful prevention? Combining methods. In one Mayo Clinic survey, 78% of people who avoided yeast infections used both a probiotic and an antifungal. Only 45% did just one.

Treatment Options: What Works, What Doesn’t
If you already have symptoms, you need treatment-not more antibiotics. That’s a common mistake. Antibiotics don’t touch yeast. Taking more just makes it worse.
- For mild cases: OTC antifungals. Clotrimazole, miconazole, or butoconazole creams or suppositories work in 80-90% of cases within 7 days. Use the full course-even if the itching stops after day two.
- For stubborn or recurrent cases: Fluconazole (Diflucan). A single 150mg pill often clears it up. For recurrent infections, doctors may prescribe three doses, 72 hours apart. It’s 95% effective. But here’s the catch: it’s not safe in pregnancy, especially in the second and third trimesters. The FDA warns it can increase the risk of birth defects by 4.5 times.
- For pregnant people: Boric acid suppositories. These are safe during pregnancy and work well for infections caused by non-albicans yeast strains. Use 600mg nightly for 14 days. They’re not available OTC in all places, so ask your doctor.
Fluconazole isn’t perfect. About 23% of users get headaches. 18% feel nauseous. Rarely, it can affect liver enzymes. But for most, the benefits outweigh the risks-when used correctly.
What Doesn’t Work (And Why)
There’s a lot of misinformation out there.
Yogurt on the skin? Putting plain yogurt in your vagina won’t help. The Lactobacillus in yogurt is different from the strains that live in your vagina. It doesn’t stick around. And the sugar in yogurt? It might feed yeast.
Apple cider vinegar baths? No evidence. They can irritate sensitive skin and don’t restore the right kind of bacteria.
Just waiting it out? You might get better in a week or two, but why suffer? And if you ignore it, the infection can get worse or spread. Plus, if you’re misdiagnosing yourself, you’re not treating the real problem.
When to See a Doctor
You don’t need to rush to the clinic for every itch. But call your provider if:
- Your symptoms don’t improve after 7 days of OTC treatment
- You have fever, pelvic pain, or foul-smelling discharge
- You’ve had four or more yeast infections in a year
- You’re pregnant
- You’re not sure it’s yeast
Doctors can do a simple swab test to confirm it’s yeast-not BV or an STI. That’s important. About 64% of self-diagnosed cases are wrong. Getting the right diagnosis means getting the right treatment.
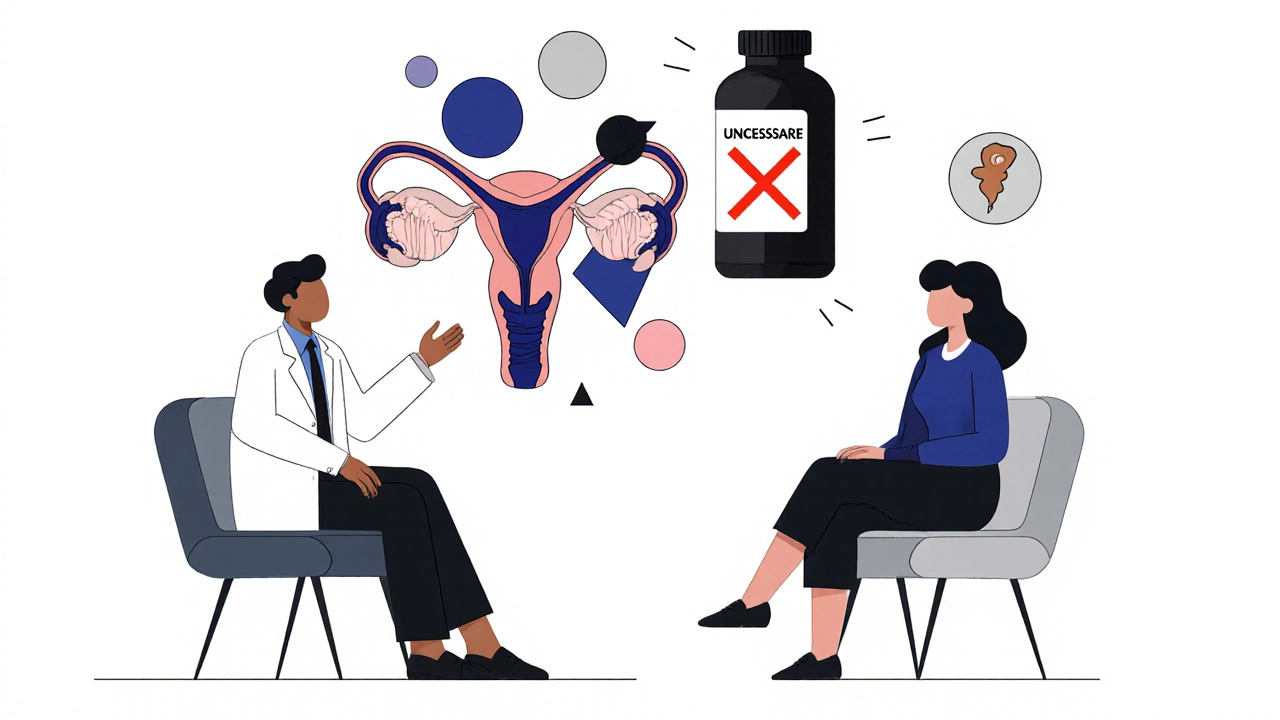
The Bigger Picture: Why This Keeps Happening
Here’s the uncomfortable truth: antibiotic overuse is a huge part of the problem. In the U.S., 30% of outpatient antibiotic prescriptions are unnecessary. That’s 236 million prescriptions a year that don’t help-and might hurt. Every one of them increases the risk of yeast infections, antibiotic resistance, and gut problems.
And yet, vaginal health research gets barely 2.5% of the NIH’s $43 billion budget. That’s why there are no official guidelines for preventing yeast infections after antibiotics. Most doctors don’t talk about it. Only 38% of OB-GYNs routinely advise patients. But 89% of patients want to know.
It’s not just about cream and pills. It’s about changing how we think about women’s health. We need better research, better education, and better access to prevention tools.
What’s Next?
Scientists are working on new solutions. Vaginal microbiome transplants-basically, giving someone a healthy vaginal microbiome from a donor-are in early trials. pH-regulating tampons are being tested. But these won’t help if we don’t fix the root problem: unnecessary antibiotics and lack of awareness.
The best defense? Be informed. Ask your doctor: "Is this antibiotic really necessary?" If it is, ask: "Should I take a probiotic or antifungal with it?" Don’t wait until you’re suffering. Prevention is simple, safe, and effective.
Can antibiotics cause yeast infections in men?
Yes, though it’s less common. Men can get penile yeast infections, especially if they have diabetes, are uncircumcised, or have unprotected sex with someone who has a yeast infection. Antibiotics can disrupt the skin’s natural bacteria, allowing Candida to overgrow. Symptoms include redness, itching, and a white discharge under the foreskin. Treatment is the same: antifungal creams like clotrimazole. Prevention includes keeping the area dry and avoiding tight clothing.
How long after antibiotics can a yeast infection develop?
Yeast infections can start as early as 2-3 days after beginning antibiotics, but most appear between days 5 and 10. This is when the Lactobacillus population drops low enough for yeast to take over. If you’re on a 7-day course, symptoms often show up right after you finish. That’s why starting prevention on day one matters.
Are probiotics better than antifungals for prevention?
They’re not better-they’re better together. Probiotics help restore balance over time. Antifungals stop yeast from growing right away. One study showed that using both reduced yeast infections by 78%, while using only probiotics lowered risk by 50%. For high-risk people, combining them is the gold standard.
Can I use yogurt as a probiotic to prevent yeast infections?
Eating plain, unsweetened yogurt with live cultures may help your gut microbiome, but it won’t prevent vaginal yeast infections. The Lactobacillus strains in yogurt (like L. acidophilus) are different from the ones that protect the vagina (like L. rhamnosus GR-1). Yogurt doesn’t colonize the vaginal tract. Stick to vaginal-specific probiotic supplements if you want real protection.
Is it safe to take fluconazole while on antibiotics?
Yes, fluconazole is safe to take with most antibiotics. There are no major drug interactions. But if you’re on antibiotics that affect the liver-like erythromycin or certain antifungals-your doctor may monitor your liver enzymes. Always tell your provider what else you’re taking. Fluconazole is not safe in pregnancy, especially in the second and third trimesters.
If you’ve ever had a yeast infection after antibiotics, you know how disruptive it is. But you don’t have to accept it as unavoidable. With the right tools-antifungals, probiotics, smart habits-you can protect yourself. And if you’re prescribed antibiotics, ask questions. Your health deserves more than silence.

Conor McNamara
November 17, 2025 AT 15:48so u know antibiotics are just part of the big pharma plan to make us sick so we buy more drugs right? they wipe out good bacteria on purpose so u get yeast infections and then u gotta buy antifungals lol. and probiotics? nah they sell those too. it's all a cycle. they don't want u healthy, they want u dependent. check the patents. it's all connected.
steffi walsh
November 17, 2025 AT 19:15OMG YES I HAD THIS AFTER MY SINUS ANTIBIOTICS 😭 I WAS SO ITCHY AND FRUSTRATED. I STARTED THE MONISTAT 7-DAY AND A FEM-DOPHILUS AND IT WAS A GAME CHANGER. YOU'RE NOT ALONE!! 💪💖
Leilani O'Neill
November 17, 2025 AT 23:10Of course you’re having yeast infections. You’re clearly not managing your lifestyle properly. Cotton underwear? That’s basic hygiene, not some miracle cure. And probiotics? If you can’t maintain a balanced diet and avoid sugar, you deserve every itch. This isn’t rocket science-it’s elementary self-discipline.
Riohlo (Or Rio) Marie
November 19, 2025 AT 00:36Let’s be real-this entire discourse is a performative wellness theater. The real issue isn’t antibiotics or probiotics-it’s the commodification of vaginal health by corporations selling ‘female empowerment’ in pill form. You think L. rhamnosus GR-1 is magic? It’s just another SKU in a billion-dollar industry that profits from your discomfort. The real cure? Stop treating your body like a broken appliance needing a fix. But of course, you’d rather buy another cream than question the system.
Emanuel Jalba
November 20, 2025 AT 05:36THIS IS WHY I WON'T TAKE ANTIBIOTICS UNLESS I'M DYING 😤 I SAW A DOCTOR FOR A COUGH LAST YEAR AND HE PRESCRIBED AMOXICILLIN. I SAID NO. I TOOK ECHINACEA, VITAMIN C, AND A HOT BATH. I'M STILL HERE. AND NO YEAST INFECTION. PEOPLE NEED TO STOP TRUSTING DOCTORS. THEY'RE ALL IN THE POCKET OF BIG PHARMA 🤬💊
Heidi R
November 20, 2025 AT 09:41You’re all missing the point. If you’re getting yeast infections from antibiotics, you’re probably eating too much sugar, wearing synthetic underwear, and not washing properly. It’s not the drug-it’s you. Fix your habits before blaming the medicine.
Kristina Williams
November 22, 2025 AT 06:04did u know the government puts fluoride in the water to kill good bacteria? that's why everyone gets yeast infections now. and the probiotics? they're fake. the real ones are only sold in underground labs in romania. i got mine from a guy on facebook. he said the pill has a tiny qr code that proves it's real. scan it and it shows the bacteria dancing. i swear it's true.
Christine Eslinger
November 24, 2025 AT 00:14For anyone reading this and feeling overwhelmed-this isn’t about perfection. It’s about small, consistent steps. Taking a probiotic even three times a week helps. Wearing cotton underwear even half the time makes a difference. You don’t need to overhaul your life overnight. Just start with one thing. And if you’re struggling, that’s okay. You’re not failing-you’re learning. Your body is trying to heal. Be gentle with it.
Denny Sucipto
November 24, 2025 AT 06:55Man, I had a yeast infection after my last round of antibiotics and I thought I was gonna lose my mind. Then I started taking the probiotic like they said and switched to cotton undies. Not magic, but it helped. I didn’t even need the cream after that. Honestly? Just listen to your body. It’s smarter than you think. And hey-if you’re on antibiotics, ask your doc about prevention. Most don’t bring it up, but you’ve got a right to know.