The Connection between Subarachnoid Hemorrhage and Aneurysms: A Closer Look
 May, 7 2023
May, 7 2023
Understanding Subarachnoid Hemorrhage and Aneurysms
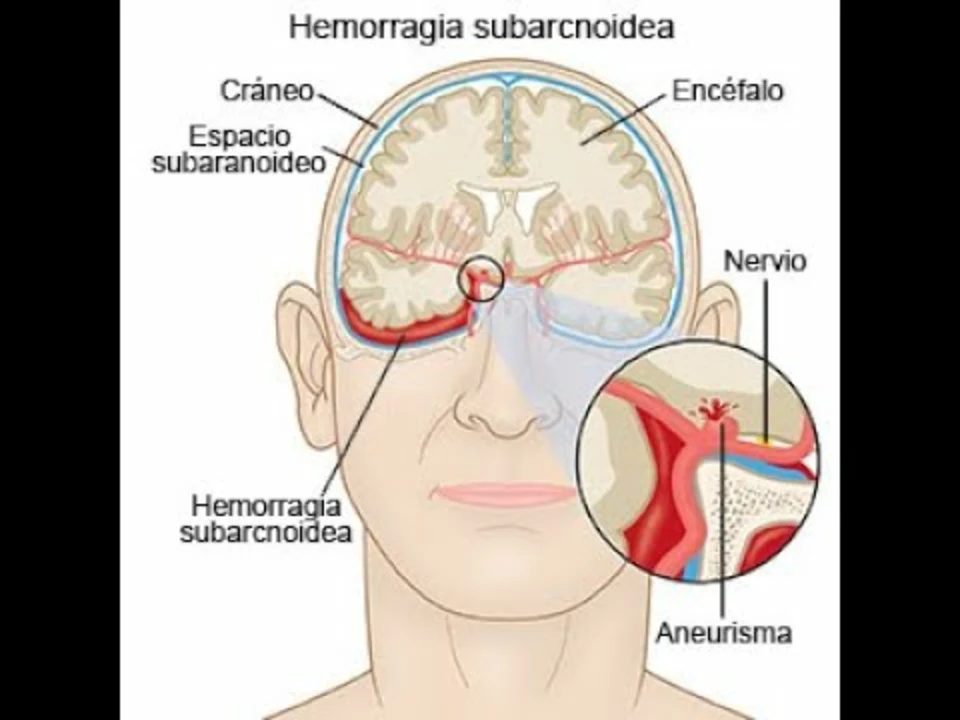
In this section, we will be discussing what Subarachnoid Hemorrhage and Aneurysms are, as well as their causes and symptoms. A Subarachnoid Hemorrhage (SAH) is a type of stroke that occurs when a blood vessel on the surface of the brain ruptures and bleeds into the space between the brain and the skull. This bleeding can cause increased pressure on the brain and damage to the surrounding tissue, leading to severe neurological damage or even death.
Aneurysms, on the other hand, are bulges in the walls of blood vessels, caused by a weakening of the vessel walls. They can occur anywhere in the body, but when they form in the brain, they are referred to as cerebral aneurysms. Cerebral aneurysms can be extremely dangerous, as they can rupture and cause a Subarachnoid Hemorrhage. In this article, we will be taking a closer look at the connection between these two conditions and discussing their diagnosis, treatment, and prevention.
Types of Aneurysms and Their Relationship with SAH
There are several types of aneurysms, and their classification depends on their shape and the location where they occur. The most common type of cerebral aneurysm is the saccular aneurysm, also known as a berry aneurysm. This type of aneurysm is characterized by a sac-like bulge in the blood vessel wall, and it is the most likely to rupture and cause a Subarachnoid Hemorrhage.
Other types of aneurysms include fusiform aneurysms, which are characterized by the widening of the entire blood vessel, and dissecting aneurysms, which occur when a tear in the blood vessel wall allows blood to flow between the layers of the vessel wall. While these types of aneurysms can also result in a Subarachnoid Hemorrhage, they are less common than saccular aneurysms.
Risk Factors for Developing Aneurysms and SAH
There are several factors that can increase a person's risk of developing an aneurysm and experiencing a Subarachnoid Hemorrhage. Some of the most common risk factors include age, family history, high blood pressure, smoking, and excessive alcohol consumption. Other risk factors include certain genetic conditions, such as polycystic kidney disease and connective tissue disorders, as well as a history of head trauma or injury.
It is important to be aware of these risk factors and make lifestyle changes to minimize the chances of developing an aneurysm and experiencing a Subarachnoid Hemorrhage. This can include quitting smoking, limiting alcohol consumption, and managing high blood pressure through medication and lifestyle changes.
Diagnosing Aneurysms and Subarachnoid Hemorrhage
Diagnosing aneurysms and Subarachnoid Hemorrhage can be challenging, as many people with aneurysms do not experience any symptoms until the aneurysm ruptures. However, there are several diagnostic tests that can be used to identify aneurysms and assess the risk of rupture. These tests may include magnetic resonance imaging (MRI), computed tomography (CT) scans, and cerebral angiography.
In the case of a suspected Subarachnoid Hemorrhage, a CT scan is usually the first diagnostic test performed, as it can quickly identify the presence of blood in the subarachnoid space. A lumbar puncture, also known as a spinal tap, may also be performed to collect cerebrospinal fluid for analysis and confirm the diagnosis.
Treatment Options for Aneurysms and SAH
The treatment of aneurysms and Subarachnoid Hemorrhage depends on the size, location, and type of aneurysm, as well as the overall health of the patient. In some cases, small, unruptured aneurysms may be monitored through regular imaging studies, and no immediate treatment may be necessary. However, if an aneurysm is determined to be at a high risk of rupture, surgical intervention may be necessary.
There are two main types of surgery used to treat cerebral aneurysms: surgical clipping and endovascular coiling. Surgical clipping involves placing a small metal clip around the base of the aneurysm to prevent blood flow into the aneurysm sac, while endovascular coiling involves inserting a catheter through an artery in the groin and guiding it to the aneurysm, where small platinum coils are released to fill the aneurysm and promote clotting. Both procedures aim to prevent the aneurysm from rupturing and causing a Subarachnoid Hemorrhage.
Managing the Aftermath of a Subarachnoid Hemorrhage
For those who have experienced a Subarachnoid Hemorrhage, the recovery process can be challenging and lengthy. It is crucial to work closely with a healthcare team, including neurologists, neurosurgeons, and rehabilitation specialists, to devise a comprehensive treatment plan. This plan may include medications to manage pain, prevent seizures, and reduce the risk of vasospasm (a dangerous narrowing of blood vessels that can occur after a Subarachnoid Hemorrhage).
Physical, occupational, and speech therapy may also be necessary to help patients regain their strength, mobility, and communication skills. Emotional support and counseling may be beneficial, as many patients experience anxiety, depression, and other emotional challenges during their recovery.
Preventing Aneurysms and Subarachnoid Hemorrhage
While it may not be possible to prevent all cases of aneurysms and Subarachnoid Hemorrhage, there are steps that can be taken to minimize the risk. Some of the most effective prevention strategies include maintaining a healthy lifestyle, managing high blood pressure, quitting smoking, and reducing alcohol consumption.
Regular check-ups with a healthcare provider can also help to identify any potential risk factors and address them before they lead to more serious health issues. In some cases, individuals with a family history of aneurysms or genetic predispositions may be advised to undergo regular imaging studies to monitor for the development of aneurysms and facilitate early intervention if necessary.

Taylor Smith
May 8, 2023 AT 13:35Big thanks for breaking this down so clearly.
Tammy Cooper
May 10, 2023 AT 03:33also why is smoking still a thing if it’s basically just a brain grenade with a delay?
Alyssa Hammond
May 11, 2023 AT 08:52Also, why do they call it a ‘berry’ aneurysm? Who thought that was cute? It’s a ticking time capsule of blood and regret.
Jill Amanno
May 12, 2023 AT 00:53And yet we keep running. We keep smoking. We keep ignoring the signs because we’re too busy proving we’re not weak. That’s the real hemorrhage.
Kate Calara
May 12, 2023 AT 12:50Chris Jagusch
May 14, 2023 AT 08:47Phillip Lee
May 16, 2023 AT 05:34Nancy N.
May 17, 2023 AT 18:18Katie Wilson
May 18, 2023 AT 14:17Shivani Tipnis
May 19, 2023 AT 12:15Cindy Fitrasari S.
May 19, 2023 AT 23:00Priyamvada Toshniwal
May 20, 2023 AT 20:14Denise Wood
May 22, 2023 AT 14:27