Switching Health Plans? How to Evaluate Generic Drug Coverage to Save Money
 Dec, 25 2025
Dec, 25 2025
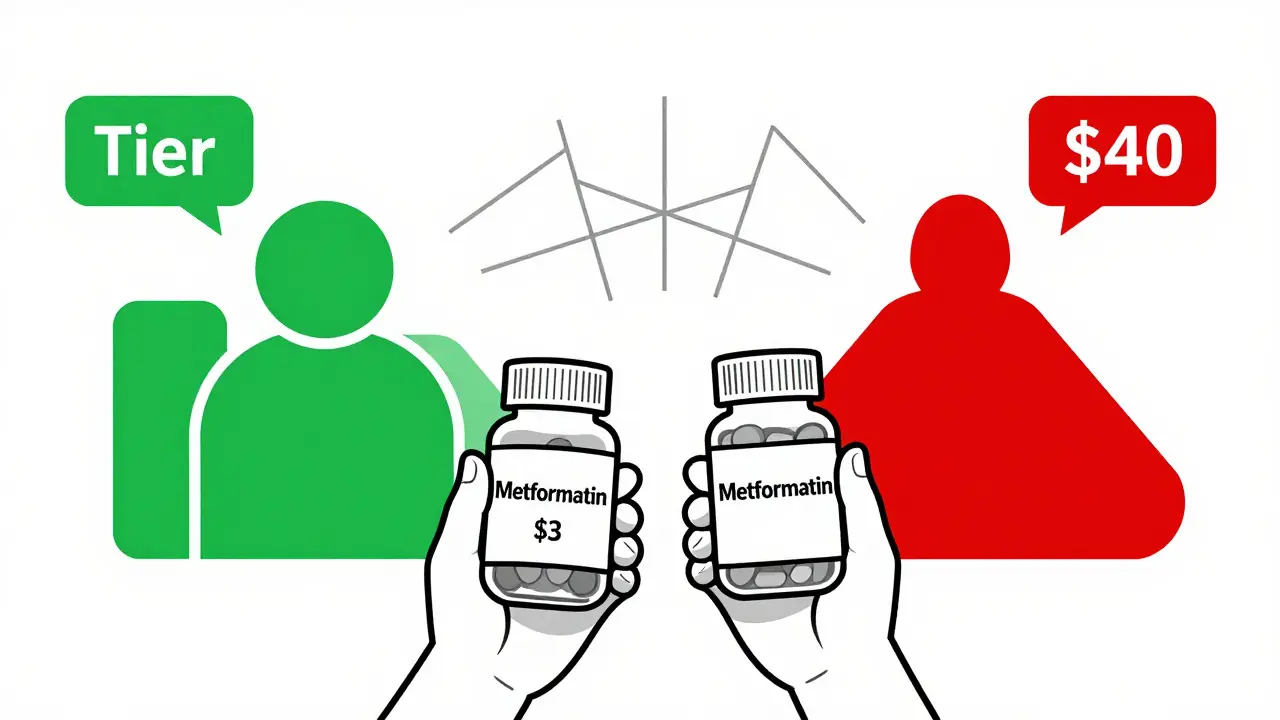
When you switch health plans, your monthly premium might drop - but your medication costs could spike. That’s because generic drug coverage isn’t the same across plans. Two plans might look identical on paper, but one could charge $3 for your blood pressure pill while the other hits you with a $40 copay. This isn’t a glitch. It’s how formularies work.
What Is a Formulary, and Why Does It Matter?
A formulary is the list of drugs your insurance covers. It’s divided into tiers, and each tier has a different price. The lowest tier - usually Tier 1 - is for generic drugs. These are chemically identical to brand-name pills but cost a fraction of the price. In 2022, generics made up 84% of all prescriptions filled, but only 14% of total drug spending. That’s the power of good coverage. But here’s the catch: not all plans treat generics the same. Some waive your deductible for Tier 1 drugs. Others make you pay the full deductible before you even see a copay. If you take three generic medications a month, that difference could cost you over $2,000 a year.Tier Structures: 3, 4, or 5? Here’s What You’re Actually Paying
Most plans use 3 to 5 tiers. The more tiers, the more confusing it gets.- 3-tier plans: Common in some employer plans. Tier 1 = generics. Copays usually $5-$10. Simple, but fewer options.
- 4-tier plans: Standard for marketplace plans under the Affordable Care Act. Tier 1 = generics ($3-$20). Tier 2 = preferred brand names. Tier 3 = non-preferred brands. Tier 4 = specialty drugs.
- 5-tier plans: Common in Medicare Advantage. Tier 1 = preferred generics ($0-$10). Tier 2 = non-preferred generics ($20-$40). Now your generic isn’t just a generic - it’s a preferred generic.
Medicare Part D vs. Marketplace Plans: Big Differences
If you’re on Medicare, your drug coverage comes through Part D. In 2023, the base deductible was $505. After that, generics typically cost $0-$10. But many plans waive the deductible entirely for Tier 1 drugs. Marketplace plans (those bought through Healthcare.gov) are different. Silver Standardized Plan Design (SPD) plans - available in 32 states as of 2024 - waive your deductible for Tier 1 generics and charge a flat $10-$20 copay. That’s huge. If you take metformin, lisinopril, and atorvastatin, you could pay $30 a month instead of $500 before coverage even starts. Non-SPD plans? You pay the full deductible - medical and prescription - before any drug coverage kicks in. So if your deductible is $3,000 and you need monthly generics, you’re paying out of pocket until you hit that number. That’s not a savings. That’s a trap.
State Rules Change Everything
Where you live matters more than you think.- In New York, generics have $0 deductible and $75 copays for specialty drugs - but regular generics? Often $0-$7.
- In California, there’s a separate $85 outpatient drug deductible. After that, you pay 20% coinsurance - capped at $250 per month.
- In Washington, D.C., you pay a $350 drug deductible, but specialty drugs are capped at $150 per script.
What You Must Check Before Switching
Don’t just look at the tier. Look at the exact drug.- Manufacturer matters. Metformin made by Teva might be Tier 1. Metformin made by Mylan might be Tier 2. Same active ingredient. Different price.
- Strength matters. Your 500mg metformin might be covered. Your 1000mg version? Not covered. Or it’s Tier 3.
- Pharmacy network matters. Your plan might cover your generic at CVS - but charge 300% more at Walgreens if it’s not in-network.
- Mail-order vs. retail. Some plans charge less if you get a 90-day supply by mail. Others don’t. Always compare.
How to Compare Plans Like a Pro
Use these tools - don’t guess.- Get the full formulary. Not just a summary. Download the PDF from the insurer’s website.
- Search your exact drugs. Type in the brand name, then the generic name, then the manufacturer and strength.
- Use a cost calculator. Medicare.gov’s Plan Finder and Healthcare.gov’s plan selector let you enter your meds and see real monthly costs. CMS says users who use these tools reduce prescription complaints by 37%.
- Calculate annual cost. Multiply your monthly copay by 12. Add any deductible you’ll pay before coverage starts. Don’t forget mail-order discounts.

Pitfalls That Cost People Thousands
Here’s what goes wrong:- Assuming all generics are equal. They’re not.
- Believing a low premium means low drug costs. Often the opposite.
- Not checking if your pharmacy is in-network. Out-of-network pharmacies can charge 400% more.
- Ignoring state rules. California’s $85 deductible? That’s real. You can’t skip it.
- Waiting until after you enroll to check. Too late.
What’s Changing in 2025?
The Inflation Reduction Act is reshaping drug costs.- Insulin is capped at $35/month - no deductible, no coinsurance.
- By 2025, Medicare Part D has a $2,000 annual out-of-pocket cap on all drugs.
- Medicare will split generics into Tier 1 (preferred) and Tier 1+ (non-preferred) - making formularies even more complex.
- AI tools like CMS’s new “Medicare Plan Scout” are being rolled out to help people compare plans faster. In testing, they cut enrollment errors by 44%.
Final Rule: Don’t Switch Without a List
Before you switch:- Write down every drug you take - brand name, generic name, manufacturer, strength, and how often.
- Check the formulary for every plan you’re considering.
- Use the official cost calculator - not the insurer’s marketing page.
- Call your pharmacy and ask: “If I switch to Plan X, what will my copay be for [your drug]?”
Are all generic drugs covered the same across health plans?
No. Two plans might both cover metformin, but one places it on Tier 1 with a $3 copay, while another puts it on Tier 2 with a $25 copay. The difference comes down to which manufacturer the insurer negotiated with, not the drug’s effectiveness. Always check the exact brand name and manufacturer on the formulary.
Do I need to meet my deductible before generic drugs are covered?
It depends on your plan. Silver Standardized Plan Design (SPD) marketplace plans waive the deductible for Tier 1 generics - you pay a fixed copay instead. Most other plans, including high-deductible health plans (HDHPs), require you to meet your full medical and prescription deductible before any drug coverage kicks in. Always read the fine print.
Can I switch plans mid-year to get better generic coverage?
Generally, no. You can only switch during Open Enrollment (November-December) or if you qualify for a Special Enrollment Period - like losing other coverage, moving, or having a baby. Exceptions are rare. Don’t wait until you’re paying too much - check your options before your plan renews.
Why is my generic drug suddenly more expensive after switching plans?
Your medication may have moved from a preferred generic (Tier 1) to a non-preferred generic (Tier 2) because the insurer changed its contract with the manufacturer. Even if the active ingredient is the same, different manufacturers are treated differently. Always verify your exact drug’s tier and manufacturer before switching.
What if my plan doesn’t cover my generic at all?
You can request a formulary exception. Contact your insurer and ask for a coverage determination. You’ll need a letter from your doctor explaining why you need that specific drug. If denied, you can appeal. Some plans also offer a transition refill - allowing you to keep your current medication for 30-90 days while you find an alternative.
How do I know if a pharmacy is in-network for my plan?
Check your plan’s website for a pharmacy directory. Call the pharmacy and ask if they accept your insurance. Don’t rely on your plan’s online tool alone - some are outdated. Out-of-network pharmacies can charge 300-400% more for the same generic drug.
Is it better to get my generics through mail-order or retail pharmacy?
Mail-order often costs less - especially for maintenance drugs. Many plans offer a 90-day supply at a lower copay than three 30-day retail fills. But some plans don’t cover mail-order at all, or charge extra for shipping. Compare the total cost for a 90-day supply versus three monthly fills before deciding.

Ryan Cheng
December 26, 2025 AT 09:15Just switched plans last year and got burned by this exact thing. My lisinopril went from $3 to $35 overnight. Didn't even realize the manufacturer changed until I got the bill. Always check the manufacturer, not just the generic name. Huge mistake.
wendy parrales fong
December 26, 2025 AT 22:37It’s wild how something so simple-like a pill-can turn into a financial maze. I used to think insurance was about helping people. Turns out it’s more like a puzzle where the pieces keep moving. But hey, at least we’re learning, right?
Jeanette Jeffrey
December 28, 2025 AT 09:46Wow. So you’re telling me people actually believe insurance companies care if they live or die? Newsflash: they care about profit margins. If your drug’s on Tier 2, congrats-you’re the sacrifice. Welcome to American healthcare.
Shreyash Gupta
December 29, 2025 AT 21:30bro i use ayurvedic herbs now 🌿😂 no more pills no more drama. my grandma in delhi never needed a formulary. maybe we overcomplicate this?
Jay Ara
December 30, 2025 AT 13:51just checked my plan and my metformin is tier 1 at $2.50. i didnt even know to look. thanks for the heads up. saved me like 500 bucks this year. you guys are lifesavers
SHAKTI BHARDWAJ
December 31, 2025 AT 05:00OMG I JUST REALIZED MY ATORVASTATIN JUST WENT TO TIER 3??? I’M GOING TO CRY IN THE PHARMACY LINE AGAIN 😭😭😭 WHY DOES THIS ALWAYS HAPPEN TO ME???
Matthew Ingersoll
December 31, 2025 AT 05:50People don’t realize how much state law affects this. In Texas, you might get lucky. In California? You’re paying a separate deductible even for generics. It’s not just the plan-it’s the state you live in. Always check both.
carissa projo
January 1, 2026 AT 14:50I used to think generics were just cheaper versions of brand names. Then I learned they’re chemically identical-same active ingredient, same safety profile, same results. The only difference? Who made it and how much the insurer paid them to be on Tier 1. It’s not about quality. It’s about corporate deals. And we’re the ones paying the price.
It’s frustrating, but knowledge is power. Once you start digging into formularies, you see the whole system for what it is: a game of financial chess. And you’ve got to play smart.
I keep a spreadsheet now. Brand name, generic, manufacturer, strength, tier, copay, mail-order option. It’s obsessive. But my wallet thanks me.
And yes, the 90-day mail-order trick? Total game-changer. My 30-day copay was $18. Mail-order? $12 for 90 days. That’s $72 saved a year. Just because I didn’t assume.
Don’t wait until you’re drowning in bills to learn this stuff. Do it now. Your future self will hug you.
josue robert figueroa salazar
January 1, 2026 AT 19:51Same drug. Different tier. Same pill. Different price. Welcome to America.
david jackson
January 2, 2026 AT 11:31Okay, so imagine this: you’ve been taking the same blood pressure pill for 8 years. Same bottle. Same pharmacy. Same life. Then one day, your insurance company switches manufacturers. Not because yours was bad. Not because it’s unsafe. But because they got a better deal with someone else. Suddenly, your $5 copay becomes $40. You’re not getting a better drug. You’re not getting a worse drug. You’re getting the exact same chemical. But now you’re paying 8x more. And you didn’t even get a vote. You didn’t even get a notice. You just woke up with a $500 surprise bill. And the worst part? The person on the other end of the phone says, ‘I’m sorry, but that’s how the formulary works.’ Like it’s some natural law. Like gravity. But it’s not. It’s a contract. A corporate contract. And you’re the one stuck holding the bag. And we’re supposed to be grateful because the premium went down $10 a month? No. No, no, no. This isn’t healthcare. This is a rigged system. And if you don’t check your formulary before switching, you’re not being careful-you’re being naive.
Jody Kennedy
January 3, 2026 AT 18:19Just used the Medicare Plan Finder and saved myself $900/year. Seriously, if you’re on meds, spend 20 minutes on that tool. It’s free. It’s accurate. It’s life-changing. Stop guessing. Start calculating.
christian ebongue
January 3, 2026 AT 23:39lol i thought tier 1 meant 'first choice' not 'first choice of the insurance company's accountant'
jesse chen
January 4, 2026 AT 06:30Just wanted to add: if you’re on a high-deductible plan, and your meds are Tier 2 or higher, you might want to ask your doctor about switching to a different generic-or even a brand if it’s cheaper after deductible. I had a patient who paid $180/month for his generic until we switched to the brand that was covered pre-deductible. He saved $1,200. Crazy, right? But it happens.