St. John’s Wort and Prescription Drugs: What You Need to Know About Dangerous Interactions
 Dec, 4 2025
Dec, 4 2025
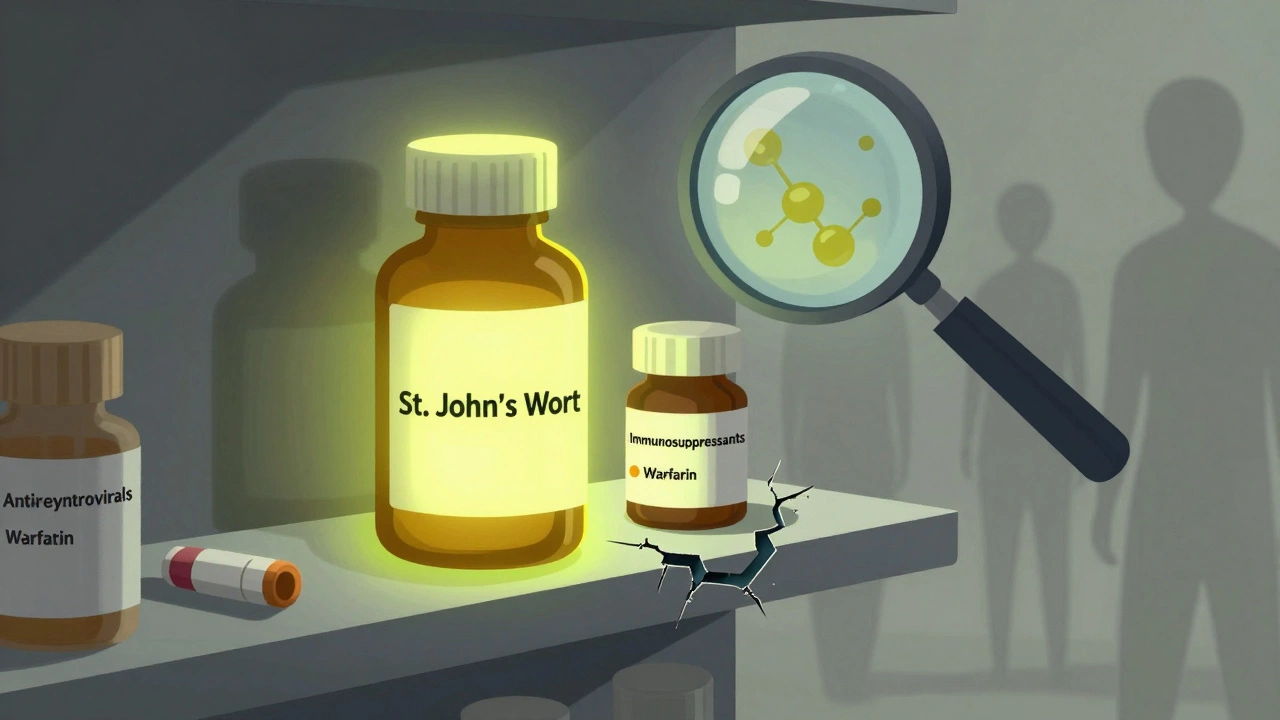
St. John’s Wort might seem like a harmless natural fix for low mood - and for some people, it works. But what many don’t realize is that this popular herbal supplement can quietly sabotage life-saving medications. If you’re taking anything from birth control to antidepressants to transplant drugs, St. John’s Wort could be making those pills useless - or worse, dangerous.
How St. John’s Wort Changes How Your Body Handles Medications
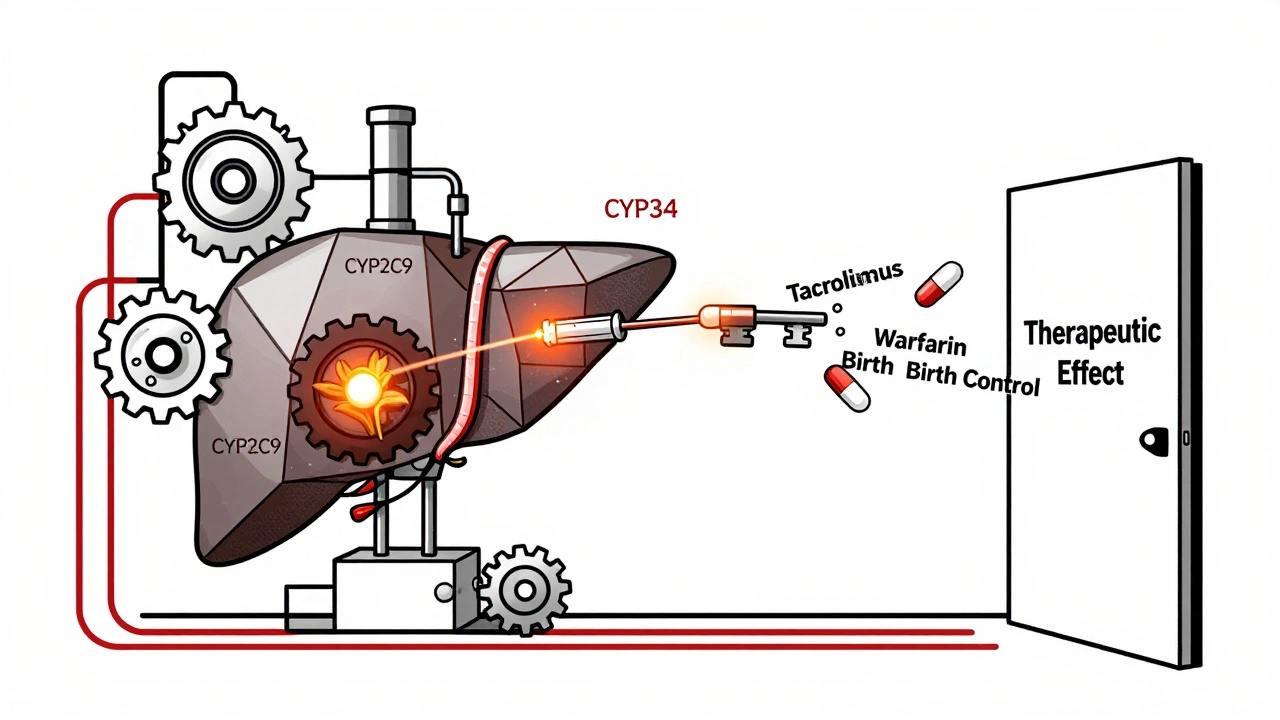
St. John’s Wort doesn’t just sit there. It actively changes how your liver and intestines process drugs. The key player is hyperforin, a compound in the plant that turns on a switch in your body called the pregnane-X-receptor. This switch tells your liver to produce more enzymes - especially CYP3A4 and CYP2C9 - that break down medications faster than normal.
Think of it like this: your prescription drug is a key trying to unlock a door. St. John’s Wort turns on a fan that blows the key away before it even gets close. The result? The drug doesn’t work.
This isn’t theoretical. In 2019, a 34-year-old woman in the U.S. had a kidney transplant and was taking tacrolimus - a drug that keeps her body from rejecting the new organ. Her levels were stable. Then she started taking St. John’s Wort for depression. Within weeks, her tacrolimus levels dropped below the safety threshold. She suffered acute organ rejection. It took emergency treatment to save her life.
Medications That Can Fail Because of St. John’s Wort
There are over 50 documented interactions between St. John’s Wort and prescription drugs. Some are common. Some are deadly.
- Immunosuppressants like cyclosporine, tacrolimus, and sirolimus - used after organ transplants - can drop to ineffective levels. This leads to organ rejection. At least 10 cases of transplant failure have been directly linked to St. John’s Wort.
- Antiretrovirals for HIV - such as indinavir and efavirenz - lose potency. Patients have seen viral loads spike, leading to drug-resistant HIV.
- Oral contraceptives become unreliable. There are dozens of documented cases of unintended pregnancies in women taking birth control pills while using St. John’s Wort. One woman reported getting pregnant after six months of using both.
- Anticoagulants like warfarin can lose their effect. A 2000 case showed a patient’s INR (a blood-clotting measure) dropped from 2.5 to 1.4 in just 10 days after starting St. John’s Wort. That’s the difference between safe blood thinning and dangerous clotting.
- Pain medications like oxycodone, methadone, and tramadol become less effective. Patients report sudden, unexplained pain returning after starting the herb.
- Antidepressants - including SSRIs like sertraline or fluoxetine - can cause serotonin syndrome when mixed with St. John’s Wort. This rare but life-threatening condition causes high fever, rapid heartbeat, confusion, and seizures.
These aren’t rare outliers. The European Medicines Agency issued warnings in 2004. The U.S. FDA issued a public advisory in 2000. Both called St. John’s Wort one of the most dangerous herbal supplements for drug interactions.

Why People Still Take It - And Why That’s Risky
It’s not hard to see why people turn to St. John’s Wort. In Germany, it’s the second most prescribed treatment for mild depression - used by about 20% of patients. Studies show it can be as effective as low-dose SSRIs for some people, with fewer side effects like weight gain or sexual dysfunction.
But here’s the catch: those benefits only matter if you’re not on any other meds. If you’re taking even one prescription drug, the risk skyrockets. A 2022 review in the Journal of Pharmacy and Pharmacology found that nearly all cases of serious interaction involved people who didn’t tell their doctor they were using the herb.
Many users assume “natural” means “safe.” But St. John’s Wort is a potent biochemical agent. It’s not tea. It’s not chamomile. It’s a drug - one that’s sold without a prescription, without safety testing, and without clear labeling.
The Delayed Danger: Why You Won’t Notice Until It’s Too Late
One of the most dangerous things about St. John’s Wort is how slowly it works - and how slowly its effects fade.
It takes about 10 days for the enzyme-inducing effect to peak. That means if you start taking it while on warfarin, you might feel fine for over a week. Then, suddenly, your blood starts clotting. No warning. No symptoms until it’s critical.
And if you stop taking St. John’s Wort? The enzyme levels don’t drop right away. They stay high for up to two weeks. So even if you quit the herb, your meds still won’t work properly for days.
A 2017 study found that the average patient took three to six weeks to connect their worsening symptoms - like breakthrough pain, unexpected pregnancy, or rejection symptoms - to the herb they’d started months earlier.
What to Do If You’re Taking St. John’s Wort
If you’re using St. John’s Wort, here’s what you need to do - right now:
- Check every medication you take. Write down every pill, patch, or injection - even over-the-counter ones. Look for any listed in the interaction list above.
- Talk to your pharmacist. Pharmacists are trained to spot these interactions. Bring your bottle of St. John’s Wort. Ask: “Could this make any of my other meds stop working?”
- Don’t stop your prescription meds cold. If you’re on warfarin, immunosuppressants, or antiretrovirals, stopping them suddenly can be deadly. Talk to your doctor first.
- Consider alternatives. If you’re using St. John’s Wort for depression, talk to your doctor about options like exercise, therapy, or SSRIs with fewer interaction risks. SAM-e and 5-HTP are other herbal options - but they have far fewer documented interactions.
There’s no safe way to combine St. John’s Wort with immunosuppressants, HIV drugs, or blood thinners. Period.
What’s Changing - And What’s Coming
Scientists are trying to fix the problem. A 2022 study tested a new version of St. John’s Wort with hyperforin removed. The result? A 90% drop in enzyme induction. That could mean a safer version in the future.
But right now, every bottle on the shelf - whether it’s from Walmart, Amazon, or a health food store - contains hyperforin. And until regulations change, you can’t trust the label to tell you what’s inside.
The global market for St. John’s Wort has dropped 37% since its peak in 2000. Sales are falling in the U.S. as more people learn the risks. But in Europe, where labeling rules are stricter, it’s still widely used - and still causing problems.
The bottom line? If you’re on any prescription medication, St. John’s Wort is not worth the risk. The benefits are limited. The dangers are real. And the consequences can be fatal.
Can I take St. John’s Wort with my antidepressant?
No. Mixing St. John’s Wort with SSRIs, SNRIs, or other antidepressants can cause serotonin syndrome - a potentially fatal condition that raises serotonin levels dangerously high. Symptoms include high fever, rapid heart rate, confusion, muscle rigidity, and seizures. Even if you feel fine at first, the risk builds over time. There is no safe dosage combination.
Does St. John’s Wort affect birth control?
Yes. St. John’s Wort speeds up the breakdown of estrogen and progestin in birth control pills, patches, and rings. This can cause breakthrough bleeding and, more seriously, unintended pregnancy. At least 17 documented cases of pregnancy occurred in women using both. If you’re on hormonal birth control, avoid St. John’s Wort entirely.
How long does St. John’s Wort stay in your system?
The herb itself clears from your body in a few days. But the enzyme-inducing effects last much longer - up to two weeks after you stop taking it. That means even if you quit St. John’s Wort, your other medications may still not work properly for 14 days. Always wait at least two weeks before starting a new drug if you’ve been using St. John’s Wort.
Is St. John’s Wort regulated like a drug?
No. In the U.S., it’s sold as a dietary supplement, so it doesn’t need FDA approval before sale. Manufacturers don’t have to prove safety, purity, or consistent potency. In Europe, labeling rules are stricter - but even there, you can’t rely on the label to warn you about all risks. The only way to know what’s in your bottle is to trust a reputable brand - and even then, hyperforin levels vary widely.
Are there safer herbal options for depression?
SAM-e and 5-HTP are two alternatives with far fewer documented drug interactions. SAM-e has minimal interactions - mainly with MAO inhibitors - and 5-HTP has very few. Neither has as much research backing for depression as St. John’s Wort, but they’re much safer if you’re on other medications. Still, talk to your doctor before starting any supplement.
What should I do if I’ve been taking St. John’s Wort with my meds?
Stop taking St. John’s Wort immediately - but don’t stop your prescription meds. Contact your doctor or pharmacist right away. Ask for blood tests to check levels of your medications (like INR for warfarin, or drug concentrations for immunosuppressants). If you’ve been using it for more than a week, you may need monitoring for up to two weeks after stopping. Don’t wait for symptoms to appear.

Emmanuel Peter
December 4, 2025 AT 10:28Ashley Elliott
December 5, 2025 AT 00:54michael booth
December 6, 2025 AT 06:41Alex Piddington
December 7, 2025 AT 02:36George Graham
December 7, 2025 AT 14:51John Filby
December 8, 2025 AT 13:52Elizabeth Crutchfield
December 9, 2025 AT 08:44Ben Choy
December 10, 2025 AT 17:29