Sleep Apnea and Cardiovascular Risk: How Breathing Problems Raise Blood Pressure and Heart Disease Danger
 Dec, 20 2025
Dec, 20 2025
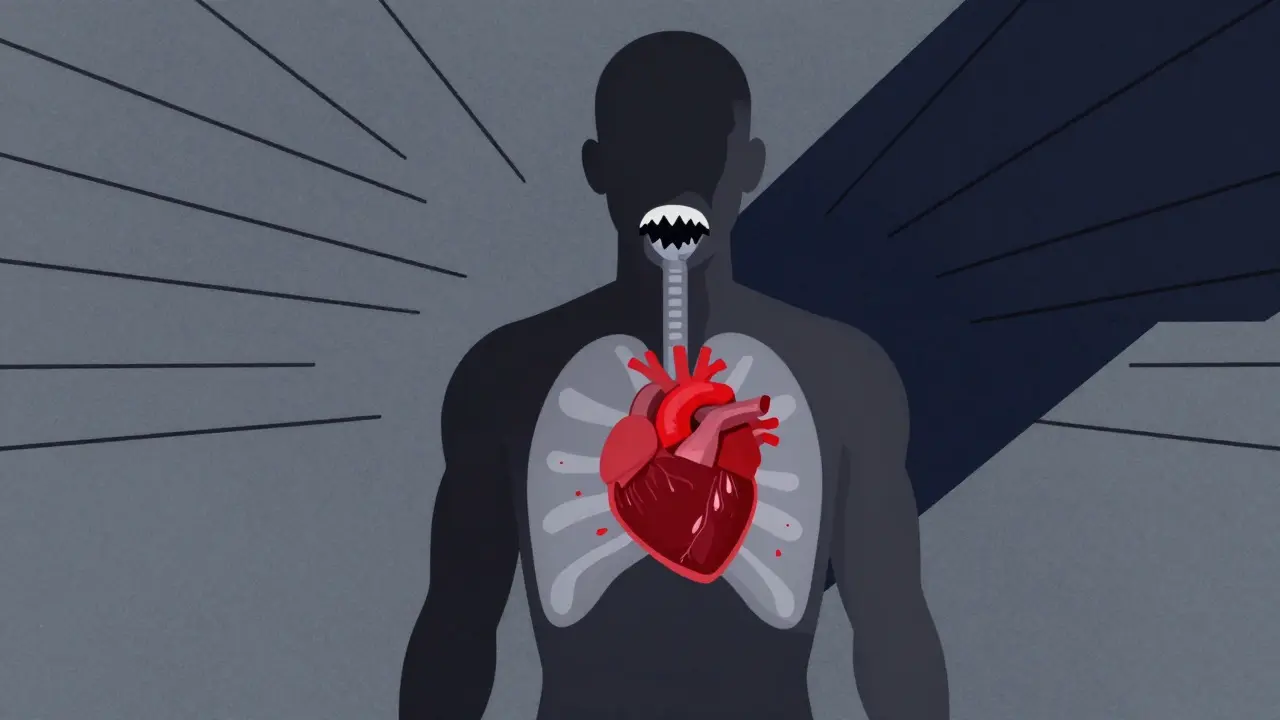
When your breathing stops at night, your heart pays the price
If you snore loudly, wake up gasping, or feel exhausted even after a full night’s sleep, you might have sleep apnea. It’s not just annoying-it’s dangerous. About 1 billion people worldwide have this condition, and most don’t even know it. In the U.S. alone, 40 million people are affected. But here’s the real concern: sleep apnea doesn’t just mess with your sleep. It directly increases your risk of high blood pressure, heart attacks, strokes, and heart failure.
The most common form, obstructive sleep apnea (OSA), happens when the muscles in your throat relax too much and block your airway. Each time this happens, your brain jolts you awake-just enough to breathe, but not enough to rest. These mini-awakenings can occur 30, 50, or even 100 times an hour. And every time, your body goes into survival mode.
Why your blood pressure spikes while you sleep
Most people expect their blood pressure to drop at night. That’s normal. But in people with sleep apnea, it doesn’t. In fact, it often rises. Up to 80% of patients with resistant hypertension-high blood pressure that won’t go down even with three different medications-have untreated sleep apnea.
Here’s why: every time your airway closes, oxygen drops. Your body responds by flooding your system with stress hormones like adrenaline. Studies show these hormone levels spike 2 to 4 times higher during sleep in people with OSA. At the same time, the effort to breathe against a blocked airway creates strong negative pressure in your chest. That forces your heart to work harder, increasing the load on your arteries by 30-50% compared to normal breathing.
The result? Your blood pressure doesn’t dip at night like it should. Instead, 70-80% of people with sleep apnea have what’s called a “non-dipping” pattern. That means their nighttime pressure stays high. This isn’t just a quirk-it’s a major red flag. People with this pattern have a much higher risk of heart attacks, strokes, and kidney damage.
How sleep apnea damages your heart over time
It’s not just about blood pressure spikes. The repeated oxygen drops and stress responses cause lasting damage. Your blood vessels start to lose their flexibility. Studies show flow-mediated dilation-a key measure of artery health-drops by 25-40% in OSA patients. That’s like having arteries that are stiff and clogged, even before plaque builds up.
Chronic inflammation is another big problem. Levels of C-reactive protein, a marker of body-wide inflammation, rise by 35-50% in people with untreated sleep apnea. Oxidative stress-damage from free radicals-also increases, with markers like malondialdehyde spiking 2 to 3 times higher than in healthy people.
All of this adds up. People with moderate to severe sleep apnea are:
- 30% more likely to develop coronary artery disease
- 140% more likely to develop heart failure
- 2.5 times more likely to have a stroke
- 4.3 times more likely to die from a stroke if their oxygen levels drop below 90% for more than 12% of the night
And the timing matters. A 2024 study of nearly 10,000 adults found that 26.5% of heart attacks in people with sleep apnea happened between midnight and 6 a.m.-a time when healthy people are least likely to have cardiac events. That’s not a coincidence. It’s the body under constant stress.
Heart failure and arrhythmias: The hidden connection
Heart failure and sleep apnea often go hand in hand. Between 40% and 60% of people with heart failure also have sleep apnea. But it’s not just a side effect-OSA makes heart failure worse. The extra strain on the heart from repeated oxygen drops and pressure swings speeds up muscle damage and weakens the pumping ability over time.
And then there’s atrial fibrillation (AFib), the most common type of irregular heartbeat. People with sleep apnea are 2 to 4 times more likely to develop AFib. In fact, nearly half of all patients with paroxysmal AFib (episodes that come and go) have undiagnosed sleep apnea-compared to just 21% of those without AFib.
Here’s the kicker: if you’ve had a procedure like catheter ablation to fix AFib, your chances of success drop by 30% if your sleep apnea isn’t treated. The same goes for cardiac resynchronization therapy-patients with untreated OSA respond 15% worse to the device.
Younger people are at higher risk than you think
Most people assume sleep apnea is an older adult problem. It’s not. A 2024 study from UT Southwestern found that adults aged 20 to 40 with sleep apnea symptoms had a 45% higher risk of high blood pressure, a 33% higher risk of diabetes, and a 25% higher risk of metabolic syndrome compared to peers without symptoms. In people over 41, the increase was only 10-12%.
This suggests sleep apnea doesn’t just add risk-it accelerates aging of the cardiovascular system. In younger adults, it’s like hitting the fast-forward button on heart disease. If you’re under 40, snoring loudly, and waking up tired, don’t brush it off as “just stress” or “poor sleep.” It could be the root cause of problems you haven’t even started to see yet.
Why treatment often fails-and what actually works
The go-to treatment for sleep apnea is CPAP: a mask that blows air into your airway to keep it open. It’s effective, but only if you use it. And here’s the problem: only 46% of people stick with it long-term. Most stop because the mask feels uncomfortable, it’s noisy, or they forget to wear it.
Here’s the truth: CPAP doesn’t always lower blood pressure dramatically. On average, it reduces systolic pressure by just 2-3 mmHg. But that doesn’t mean it’s not working. It reduces stroke recurrence by 37%, improves heart failure outcomes, and cuts the risk of fatal heart events significantly.
For people with heart failure and central sleep apnea (a less common type caused by brain signaling issues), CPAP can be life-saving. But for others, alternatives like oral appliances, weight loss, or positional therapy (sleeping on your side) may help.
The real breakthrough isn’t just treatment-it’s detection. The American Heart Association now recommends that all patients with high blood pressure, AFib, stroke, or heart failure be screened for sleep apnea. Simple tools like the STOP-Bang questionnaire (which asks about snoring, tiredness, observed apneas, blood pressure, BMI, age, neck size, and gender) have an 84% sensitivity for spotting moderate to severe cases.

What you should do if you suspect sleep apnea
If you have any of these, talk to your doctor:
- Snoring that wakes you or your partner
- Waking up gasping or choking
- Daytime fatigue even after 8 hours of sleep
- High blood pressure that won’t respond to medication
- Diagnosed with heart disease, AFib, or stroke
Don’t wait for a sleep study to be scheduled. Ask about a home sleep test. These are 85-90% accurate for moderate to severe cases. If it’s positive, follow up with a sleep specialist. If it’s negative but you still have symptoms, ask for a full overnight sleep study in a lab.
And if you’re overweight-especially with a neck size over 17 inches for men or 16 inches for women-losing even 10% of your body weight can cut apnea episodes in half.
Cardiologists are now looking at your sleep
For years, sleep apnea was seen as a pulmonologist’s problem. Now, cardiologists are making it part of routine care. Why? Because treating sleep apnea isn’t just about better sleep-it’s about saving lives. Untreated OSA undermines every other heart treatment you’re getting. Medications, stents, ablations, devices-they all work less well if your breathing is still failing at night.
Integrated care is the future. That means your cardiologist, sleep specialist, and primary doctor working together. It means screening for sleep apnea before you get an ablation. It means checking your blood pressure pattern, not just your daytime numbers.
Sleep apnea is not a minor inconvenience. It’s a silent cardiovascular killer. And it’s more common than most people realize. If you have heart disease, high blood pressure, or unexplained fatigue, your sleep might be the missing piece.
Key takeaways
- Up to 80% of people with resistant high blood pressure have undiagnosed sleep apnea.
- Obstructive sleep apnea increases heart failure risk by 140% and stroke risk by 2.5 times.
- Heart attacks in people with sleep apnea are more likely to happen between midnight and 6 a.m.
- Young adults with sleep apnea face a much higher risk of early heart disease than older adults.
- CPAP reduces stroke recurrence by 37% and improves heart failure outcomes-even if blood pressure drops only slightly.
- Screening with tools like STOP-Bang is simple, fast, and should be routine for heart patients.

Erika Putri Aldana
December 20, 2025 AT 14:39Swapneel Mehta
December 21, 2025 AT 12:18Jay lawch
December 21, 2025 AT 14:01Christina Weber
December 22, 2025 AT 13:13mukesh matav
December 24, 2025 AT 01:44Peggy Adams
December 24, 2025 AT 17:45Sarah Williams
December 26, 2025 AT 16:56Dan Adkins
December 27, 2025 AT 09:12Grace Rehman
December 29, 2025 AT 02:15Siobhan K.
December 29, 2025 AT 23:21Brian Furnell
December 30, 2025 AT 17:17Southern NH Pagan Pride
December 31, 2025 AT 03:56Orlando Marquez Jr
December 31, 2025 AT 13:15Jackie Be
January 2, 2026 AT 12:07John Hay
January 4, 2026 AT 08:09