Safe Migraine Treatments During Pregnancy and Lactation: What Works Without Risk
 Jan, 6 2026
Jan, 6 2026
When you’re pregnant or breastfeeding, every medication you take feels like a gamble. You want relief from migraine pain, but you also don’t want to risk your baby’s health. The truth is, you don’t have to choose between suffering and safety. Many effective, safe options exist - if you know what they are.
Migraines affect up to 1 in 5 women of childbearing age. For many, symptoms improve during pregnancy thanks to rising estrogen levels. But for others, they get worse - especially after delivery when hormones crash. Left untreated, migraines aren’t just painful. They raise your risk of preterm birth, preeclampsia, and low birth weight. The real danger isn’t the meds - it’s the pain itself.
Start with What’s Natural
Before you reach for a pill, try the non-drug approaches that work just as well - and carry zero risk. The American College of Obstetricians and Gynecologists and the American Headache Society both recommend these as first-line treatments.
- Get 7 to 9 hours of sleep every night. Irregular sleep is one of the top migraine triggers.
- Move your body 30 minutes a day, 5 days a week. Walking, swimming, or prenatal yoga can cut migraine frequency by up to 40%.
- Stay hydrated. Drink 2 to 3 liters of water daily. Dehydration is a silent migraine trigger most women overlook.
- Eat small, balanced meals every 3 to 4 hours. Low blood sugar can spark an attack.
- Try acupuncture. A 2021 study of 120 pregnant women found 68% had at least a 50% drop in migraine days after 8 weekly sessions with a certified practitioner.
- Use massage therapy. Two 30-minute sessions per week in the second and third trimesters reduced migraine frequency by 35% in one 2020 study.
- Try biofeedback. With consistent practice (3-5 times a week), this technique helps you control stress responses and cuts migraine frequency by 40-60%.
- Consider the Cefaly device. This FDA-cleared headband stimulates nerves to prevent migraines. In studies, 68% of users saw at least half fewer attacks - and it’s safe during pregnancy and breastfeeding.
These aren’t just "nice to have" tips. They’re clinically proven tools that reduce the need for meds. Many women find they can avoid drugs entirely by sticking to this routine.
Acute Relief: What You Can Take Safely
If a migraine hits and you need fast relief, here’s what’s safe - backed by data from thousands of pregnancies and breastfeeding infants.
Acetaminophen (Tylenol) is your go-to. It’s the most studied and safest option during pregnancy. Take up to 3,000 mg per day - that’s six 500 mg tablets. No link to birth defects. No increased risk of miscarriage. No harm to breastfed babies. The Relative Infant Dose (RID) is just 8.81%, far below the 10% safety cutoff.
Ibuprofen (Advil, Motrin) is also safe - but only in the first two trimesters. Avoid it after 30 weeks because it can affect fetal circulation. During breastfeeding, it’s one of the safest NSAIDs. Its RID is only 0.65%. Most babies show no side effects.
Sumatriptan (Imitrex) is the most studied triptan in pregnancy. Three large studies involving over 1,200 pregnancies found no increase in birth defects beyond the normal 3% baseline. It’s also safe for breastfeeding. The RID is just 3.0%. To be extra cautious, take it right after nursing and wait 3-4 hours before the next feeding. This lets most of the drug clear from your system.
Rizatriptan (Maxalt) has less data but shows a very low RID of 1.2%. It’s considered likely safe based on its pharmacokinetics.
Other options: Diphenhydramine (Benadryl) - RID 3.5%, metoclopramide (Reglan) - RID 0.5%, and ondansetron (Zofran) - RID 0.7% are all L2 classified, meaning they’re compatible with breastfeeding. These help if nausea comes with your migraine.
What to avoid? Ergots like ergotamine can cause dangerous uterine contractions and are linked to fetal limb defects. Valproic acid (Depakote) raises the risk of neural tube defects by 11%. Feverfew, a herbal remedy, increases miscarriage risk by 38%.
Preventing Migraines: What’s Safe Long-Term
If you get migraines often - three or more days a month - you may need daily prevention. Not all preventives are safe during pregnancy or breastfeeding.
Magnesium is your best bet. Take 400-600 mg daily in the form of magnesium citrate or glycinate. A 2021 Cochrane Review of 550 pregnant women found it reduced migraine frequency by 35% with zero side effects to mom or baby.
Riboflavin (Vitamin B2) - 400 mg daily - has shown promise in small studies. It’s naturally found in eggs and dairy, and no harm has been reported. While large-scale data is still limited, it’s considered L1 (safest) for breastfeeding.
Propranolol is sometimes used for prevention. It crosses into breast milk at low levels (RID 0.3-0.5%), but watch your baby for signs of drowsiness or slow heart rate. In pregnancy, it’s linked to a 15% higher risk of slow fetal growth and small placenta. Use only if benefits clearly outweigh risks.
Cyclobenzaprine (a muscle relaxant) has been studied in 127 pregnancies with no major malformations reported. It’s a second-line option if other preventives fail.
Amitriptyline and sertraline are antidepressants sometimes used for migraine prevention. Their RIDs are low (1.9-2.8% and 0.4-2.2%, respectively), and they’re considered compatible with breastfeeding. They’re often chosen if you also have anxiety or depression.
Verapamil, a calcium channel blocker, has the lowest RID among this class - just 0.15-0.2%. It’s a good alternative if beta-blockers aren’t right for you.
What’s off-limits? Topiramate and valproate are linked to major birth defects. Atogepant and rimegepant (new CGRP blockers) are approved for migraine prevention, but pregnancy data is still too limited to recommend them. Rimegepant is L2 for breastfeeding, but avoid it in pregnancy unless absolutely necessary.
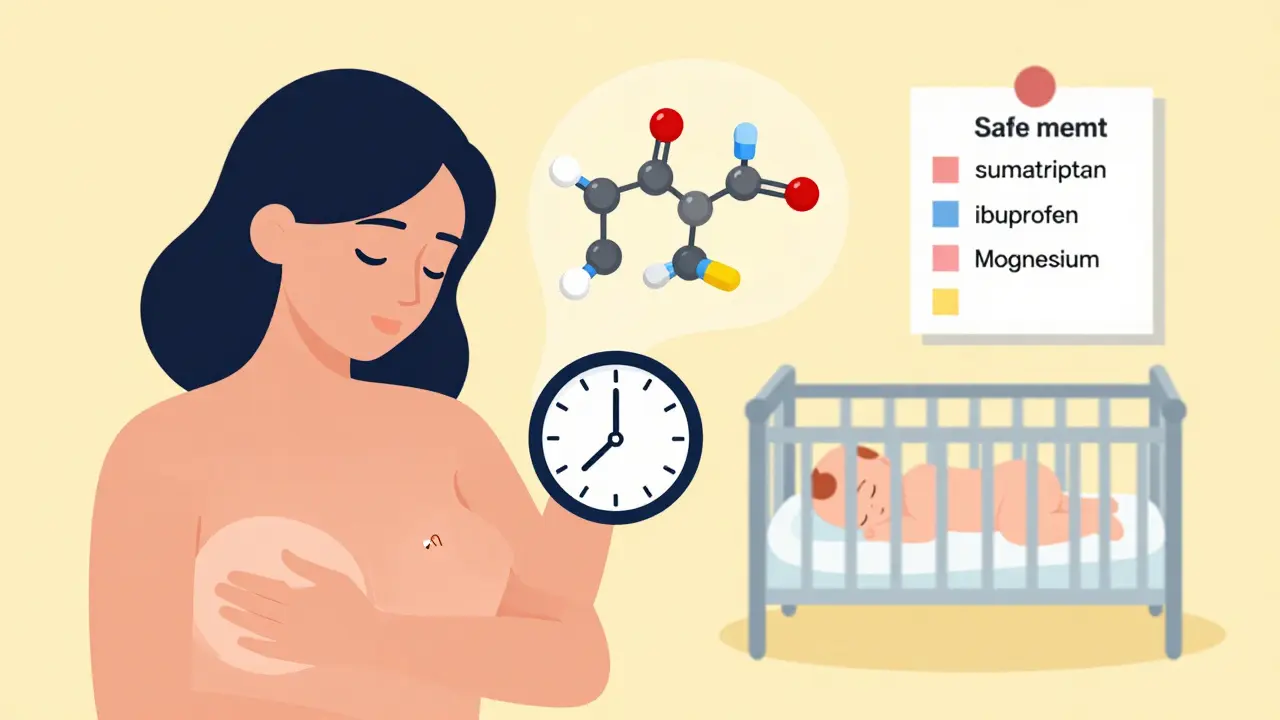
Timing Matters - Especially When Breastfeeding
If you’re nursing, timing your meds can cut your baby’s exposure by more than half. Here’s the simple rule:
- Take your medication right after you finish nursing.
- Wait 3 to 4 hours before the next feeding.
- This gives your body time to process and clear the drug.
For example, if you nurse at 7 a.m., take your sumatriptan at 8 a.m. Your next feeding can be at 12 p.m. or later. This strategy works for acetaminophen, ibuprofen, triptans, and even antidepressants.
Most moms who follow this approach report no issues with their babies. In fact, a 2023 survey of 1,247 breastfeeding mothers found 78% successfully managed migraines with acetaminophen and ibuprofen alone - and 92% of those who used triptans saw no side effects in their infants.
What Doctors Don’t Tell You
Here’s the uncomfortable truth: 42% of OB-GYNs and 68% of neurologists say they feel undertrained in managing migraines during pregnancy and breastfeeding. That means you might get outdated advice - like being told to "just tough it out" or avoid all meds.
You deserve better. Ask your doctor:
- "Is this medication safe for breastfeeding? What’s the RID?"
- "Can we try magnesium or biofeedback first?"
- "What’s the lowest dose I can use for the shortest time?"
Don’t be afraid to ask for a referral to a headache specialist or an International Board Certified Lactation Consultant (IBLCE). These professionals see hundreds of cases like yours and know exactly what works.
The Bigger Picture: Why Treating Migraines Matters
Some moms think avoiding meds is safer - but untreated migraines are worse for your baby than most medications.
Chronic pain raises your cortisol levels by 45-60%. That stress hormone crosses the placenta and affects fetal development. Sleep deprivation from migraines cuts REM sleep by 30-40%, which impacts your ability to care for your newborn. And untreated migraines increase your risk of postpartum depression by 2.7 times.
Managing your migraines isn’t selfish - it’s essential. When you feel better, you bond better, feed better, and recover faster.
What’s New in 2026
The FDA approved rimegepant (Nurtec ODT) for both acute and preventive use in 2023. It’s L2 for breastfeeding - meaning it’s likely safe. But pregnancy data is still limited, so it’s not a first choice unless other options fail.
Neuromodulation devices like gammaCore (vagus nerve stimulator) are gaining traction. In a 2021 trial, 52% of pregnant women saw a 50% drop in migraine days. The downside? Insurance still covers it for only 32% of U.S. plans.
Research is accelerating. By 2027, clinical trials focused on pregnancy and lactation safety are expected to increase by 25%. That means better data, safer options, and more confidence for moms.
You don’t have to suffer. You don’t have to guess. With the right tools - natural and medical - you can manage your migraines safely and keep your baby protected.

Poppy Newman
January 7, 2026 AT 02:32OMG this is exactly what I needed 😭 I had a migraine for 3 days postpartum and was terrified to take anything. Tried acetaminophen and it was a game-changer. Thank you for laying this out so clearly!
Adam Gainski
January 7, 2026 AT 18:51Great breakdown. I’m a neurologist and this aligns perfectly with current ACOG and AHS guidelines. A lot of providers still push "avoid all meds" out of fear, but the data is clear: untreated migraines are riskier than acetaminophen or sumatriptan when used properly. Hydration and sleep are underrated too - most patients don’t realize how big a role they play.
Anthony Capunong
January 8, 2026 AT 12:53Why are we even talking about this? In my country, we just take Tylenol and move on. You people overcomplicate everything. If you’re pregnant and in pain, you take what works. Stop being so paranoid. My wife had 3 kids and never once checked an RID. She’s fine. Baby’s fine. End of story.
Elen Pihlap
January 8, 2026 AT 18:20I tried everything. Magnesium made me diarrhea. Acupuncture was a waste of $200. Cefaly felt like a bee stung my forehead. I just want to sleep. Why does this feel so hard? I hate that my body does this to me. I miss being me.
Sai Ganesh
January 8, 2026 AT 19:23In India, many women use ginger tea and rest. No drugs. No devices. Just tradition and patience. I respect the science here, but let’s not forget that for centuries, mothers managed without all this tech. Maybe the answer is balance - modern tools + ancient wisdom.
Andrew N
January 10, 2026 AT 11:57Wait. You’re saying sumatriptan is safe? But the FDA label says "Category C". And you’re quoting RID percentages like they’re gospel? That’s not how pharmacology works. You need to look at placental transfer, fetal metabolism, long-term neurodevelopmental outcomes. You’re oversimplifying a complex issue.
LALITA KUDIYA
January 11, 2026 AT 22:27thank you for this i was so scared to ask my doc anything but now i feel empowered. magnesium changed my life. no more panic attacks when i feel a migraine coming
Jessie Ann Lambrecht
January 13, 2026 AT 21:58THIS. This is the kind of post that saves lives. I used to cry in the bathroom during my third trimester because I was too afraid to take Tylenol. Now I’m a mom of two and I’ve got my Cefaly on my nightstand like it’s my phone. You’re not weak for needing help - you’re strong for seeking it. Keep going, mama. You’re doing better than you think.
Rachel Steward
January 14, 2026 AT 17:37Let’s be real - this is all just corporate-funded placebo theater. Acetaminophen is a synthetic compound. Biofeedback? It’s just breathing with a machine. The real solution is eliminating stressors - toxic relationships, overwork, societal pressure on mothers to be perfect. Migraines are a symptom of a broken system, not a medical glitch to be patched with gadgets and pills. You’re treating the symptom, not the soul.
Anastasia Novak
January 16, 2026 AT 01:05Ugh. I read this whole thing and now I feel like I’m in a wellness influencer’s Instagram carousel. "Try acupuncture!" "Use the Cefaly!" Why is everything so expensive and performative? My grandma just drank tea and lay down. No device. No 8-step plan. Just silence. Why can’t modern medicine just be simple again?
Jonathan Larson
January 16, 2026 AT 02:17While the data presented is robust and clinically sound, I would respectfully suggest that the cultural and socioeconomic barriers to accessing these treatments - particularly neuromodulation devices and certified practitioners - are not adequately addressed. For many mothers, especially in rural or under-resourced areas, the recommendation to "try biofeedback" or "purchase a Cefaly" is not merely impractical - it is inequitable. True patient-centered care must account for access, not just efficacy.
Alex Danner
January 16, 2026 AT 09:55Just want to add - if you’re on sertraline for migraines and breastfeeding, monitor your baby’s feeding patterns. One mom in my support group noticed her baby started sleeping 6 hours straight after she started it - which sounds great until you realize she was barely waking to nurse. Low RID doesn’t mean zero impact. Watch for subtle changes. And if in doubt, talk to an IBCLC. They’re the real MVPs.