Raltegravir and Tuberculosis Co-Infection: A Comprehensive Guide
 Apr, 29 2023
Apr, 29 2023
Understanding Raltegravir and Tuberculosis Co-Infection
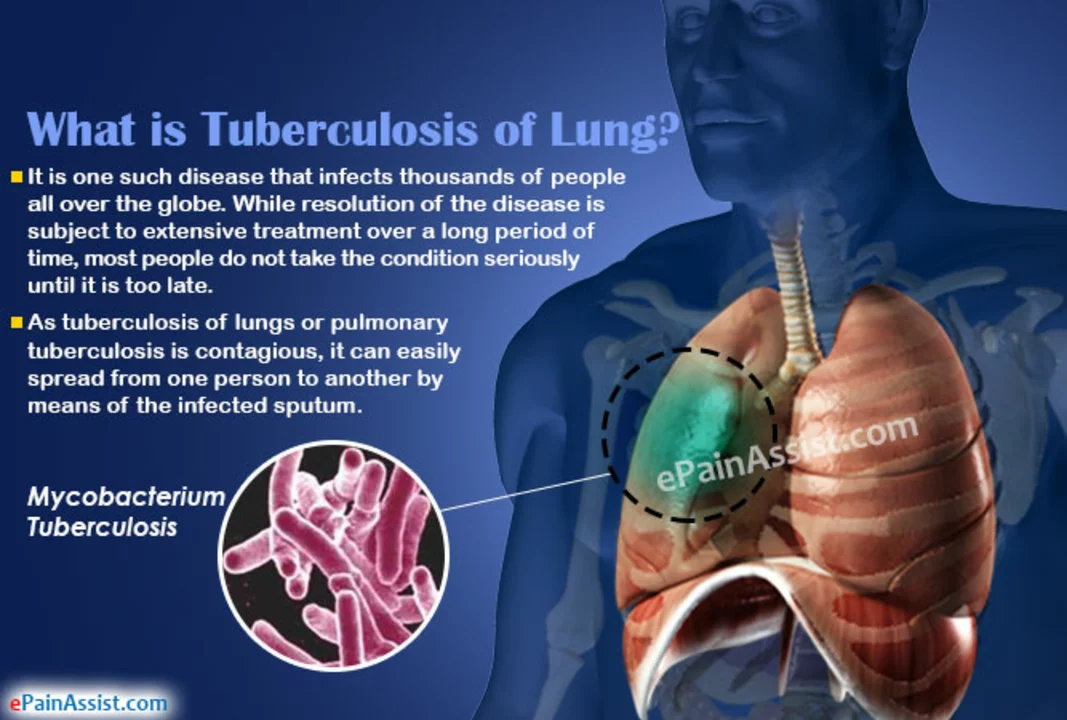
As a blogger, I feel it's important to discuss the connection between Raltegravir and Tuberculosis co-infection. Tuberculosis (TB) is a life-threatening infectious disease caused by the bacterium Mycobacterium tuberculosis. On the other hand, Raltegravir is an antiretroviral drug used in the treatment of human immunodeficiency virus (HIV) infection. In this section, I will provide a comprehensive understanding of both Raltegravir and Tuberculosis, as well as how they relate to one another as a co-infection.
For those who may be unfamiliar with these terms, HIV is a virus that attacks the immune system, leading to a weakened ability to fight infections and diseases like TB. Raltegravir, as an antiretroviral drug, helps to suppress the HIV virus and prevent it from multiplying in the body. This, in turn, helps to improve the immune system's ability to fight off infections like TB.
However, when a person becomes co-infected with both HIV and TB, the situation can become quite complex. The weakened immune system caused by HIV can make it more difficult for the body to fight off TB, leading to more severe and prolonged illness. Moreover, the medications used to treat each infection may interact with one another, necessitating careful monitoring and adjustment of treatment plans.
Signs and Symptoms of Tuberculosis and Raltegravir Side Effects
It is essential to understand the signs and symptoms of both Tuberculosis and the potential side effects of Raltegravir treatment. This way, individuals who are co-infected can quickly identify any potential issues and seek medical assistance if necessary. In this section, I will outline the typical signs and symptoms of Tuberculosis as well as potential side effects of Raltegravir.
Tuberculosis symptoms can include a persistent cough, fever, night sweats, weight loss, and fatigue. In more severe cases, patients may also experience chest pain or cough up blood. It is essential to seek medical attention if you suspect you may have TB, as early diagnosis and treatment can significantly improve outcomes.
As for Raltegravir, some common side effects may include nausea, diarrhea, headache, and fatigue. More severe side effects can include severe skin reactions, liver problems, and severe allergic reactions. It is crucial to discuss any potential side effects with your healthcare provider and report any new or worsening symptoms immediately.
Diagnosing and Treating TB in HIV-Positive Patients
Diagnosing and treating TB in HIV-positive patients can be a complex process, as the weakened immune system can lead to atypical presentations and complications in treatment. In this section, I will discuss the importance of early diagnosis and the various treatment options available for TB in individuals co-infected with HIV.
Early diagnosis of TB is crucial in HIV-positive patients, as the weakened immune system can lead to more severe and disseminated forms of the disease. Healthcare providers may use a combination of tests, such as sputum culture, chest X-ray, and blood tests, to diagnose TB in these patients.
Treatment for TB in HIV-positive patients typically involves a combination of medications, often including Raltegravir as part of the antiretroviral therapy. Additionally, patients may receive anti-TB medications like isoniazid, rifampin, pyrazinamide, and ethambutol. It is essential to follow the prescribed treatment plan and communicate with your healthcare provider regularly to ensure optimal outcomes.
Drug Interactions Between Raltegravir and Anti-TB Medications
As mentioned earlier, one of the challenges in treating co-infected patients is the potential for drug interactions between Raltegravir and anti-TB medications. In this section, I will discuss some of the known interactions and the importance of close monitoring and communication with healthcare providers to avoid potential complications.
One of the most significant interactions is between Raltegravir and rifampin, a commonly used anti-TB medication. Rifampin can decrease the effectiveness of Raltegravir, which may lead to reduced HIV suppression and potential treatment failure. As a result, healthcare providers may need to adjust the dosing of Raltegravir or consider alternative medications to avoid this interaction.
It is crucial for patients to disclose all medications they are taking, including over-the-counter drugs, supplements, and herbal remedies, to their healthcare provider. This allows for proper monitoring and adjustment of treatment plans to ensure the best possible outcomes.
Monitoring and Follow-Up Care for Co-Infected Patients
Regular monitoring and follow-up care are essential for patients co-infected with HIV and TB, as it helps to ensure the effectiveness of treatment and identify any potential complications early. In this section, I will discuss what to expect during follow-up appointments and the importance of adhering to the recommended monitoring schedule.
During follow-up appointments, healthcare providers will assess the patient's response to treatment, evaluate any potential side effects or drug interactions, and adjust the treatment plan as necessary. This may involve blood tests, imaging studies, and physical examinations to monitor the patient's overall health and response to therapy.
It is crucial for patients to attend all scheduled follow-up appointments and communicate any concerns or changes in symptoms to their healthcare provider. This allows for the best possible care and the greatest chance of successful treatment outcomes.
Preventing TB in HIV-Positive Patients
Preventing TB in HIV-positive patients is a crucial aspect of managing co-infections, as the weakened immune system can make individuals more susceptible to developing TB. In this section, I will discuss various strategies for preventing TB in HIV-positive patients, including preventive therapy and lifestyle modifications.
Preventive therapy, also known as isoniazid preventive therapy (IPT), involves taking the anti-TB medication isoniazid for a prescribed period to prevent the development of active TB. This therapy is recommended for individuals with a high risk of developing TB, including those with HIV.
Additionally, lifestyle modifications such as maintaining a healthy diet, exercising regularly, and avoiding exposure to individuals with active TB can help reduce the risk of developing TB in HIV-positive patients. It is also vital to adhere to the prescribed antiretroviral therapy to maintain a healthy immune system and reduce the risk of co-infections.
Living with HIV and TB Co-Infection: Tips for Success
Managing HIV and TB co-infection can be challenging, but with the right treatment plan and support, individuals can lead healthy and fulfilling lives. In this section, I will provide some tips for success in living with HIV and TB co-infection, including medication adherence, emotional support, and self-care.
Adherence to the prescribed treatment plan is crucial for successful outcomes in managing both HIV and TB. This includes taking all medications as directed, attending follow-up appointments, and communicating with healthcare providers about any concerns or changes in symptoms.
Emotional support from friends, family, and support groups can also play a significant role in coping with the challenges of co-infection. Connecting with others who understand your experiences can provide valuable encouragement and advice.
Lastly, practicing self-care through maintaining a healthy lifestyle, managing stress, and seeking mental health support when needed can help individuals living with HIV and TB co-infection to thrive in their daily lives.

Andrew Butler
April 29, 2023 AT 21:02Look, if you're on Raltegravir and you get TB, you better believe the rifampin interaction is gonna mess you up. I've seen it in the literature-CYP3A4 induction, plasma concentrations of raltegravir plummet like a rock. You think your ART is working? It's not. You need to switch to dolutegravir or adjust the dose to 1200mg BID. No exceptions. This isn't a suggestion, it's clinical fact. Stop winging it with TB treatment in HIV+ folks.
And for the love of god, stop calling it 'co-infection' like it's some cute little combo. It's a lethal synergy. TB is the silent killer, HIV is the enabler. Together? They're a death sentence without proper monitoring. Get your labs. Get your chest X-rays. Stop being lazy.
Varun Gupta
April 30, 2023 AT 07:38bro tb and hiv are just big pharma's way to sell more pills 😏
they don't want you cured they want you on meds forever 💊💸
what if the real cure is fasting and sunlight? 🌞
why is no one talking about this?? 🤔
Amy Reynal
April 30, 2023 AT 23:35Okay, so I'm a nurse in Atlanta and I've seen more HIV/TB co-infections than I care to count, and honestly? The biggest issue isn't the drug interactions-it's the stigma. People get diagnosed with TB and assume they're contagious monsters. They get kicked out of housing, fired from jobs, abandoned by family. Meanwhile, their HIV meds are sitting untouched because they're too ashamed to go back to the clinic.
And Raltegravir? Yeah, it's great-less hepatotoxic than efavirenz, better for pregnancy, easier on the CNS-but if your patient can't afford the bus fare to the clinic every week, none of it matters.
Also, can we PLEASE stop calling IPT 'preventive therapy' like it's optional? It's a public health lifeline. The WHO says so. The CDC says so. Your neighbor who works at the laundromat and coughs all day? She needs it. Not a 'maybe.' Not 'if you feel like it.'
And yes, I typed this on my phone. I'm tired. But I'm not stopping.
Also, I love you all. Keep showing up for your patients. Even when it's messy. Especially then.
Erick Horn
May 1, 2023 AT 00:22Typical. Another blog post pretending to help while ignoring the real problem: poverty.
Drug interactions? Please. The real interaction is between hunger and healthcare.
Also, rifampin doesn't 'decrease effectiveness.' It just exposes how little we care about people who need this.
Lidia Hertel
May 2, 2023 AT 13:08Y'all are overcomplicating this so much 😭
I work in a clinic in Manchester and we just got a guy from Nigeria with HIV and TB-he was terrified, couldn't afford the meds, spoke zero English. We got him on a fixed-dose combo, linked him to a peer navigator, and now he's laughing with the other patients over chai. 🫖❤️
It's not about the perfect drug regimen. It's about someone showing up. Saying 'I see you.' Making sure they get their pills. Helping them find a ride. Calling them on their bad days.
Raltegravir? Sure, it's great. But what's greater? A human who remembers your name.
Also, I cried reading this post. Not because it's perfect-but because it exists. Keep writing. We need more of this.
Chris Bock
May 3, 2023 AT 11:05Everything is a system.
And systems are designed to fail.
But we pretend we can fix them with pills.
How quaint.
Alyson Knisel
May 3, 2023 AT 18:41i just want to say thank you for writing this. i was diagnosed with hiv last year and then got tb this spring. i didn't know any of this stuff. i thought i was just 'sick' and that was it. reading this made me feel less alone. also, i misspelled everything here. my brain is still foggy from the meds. but i'm trying. and that counts, right?
also, if anyone else is out there struggling to take 12 pills a day and still showing up for work... you're doing better than you think.