Placebo Effect with Generics: Why Perception Shapes Medication Outcomes
 Jan, 26 2026
Jan, 26 2026
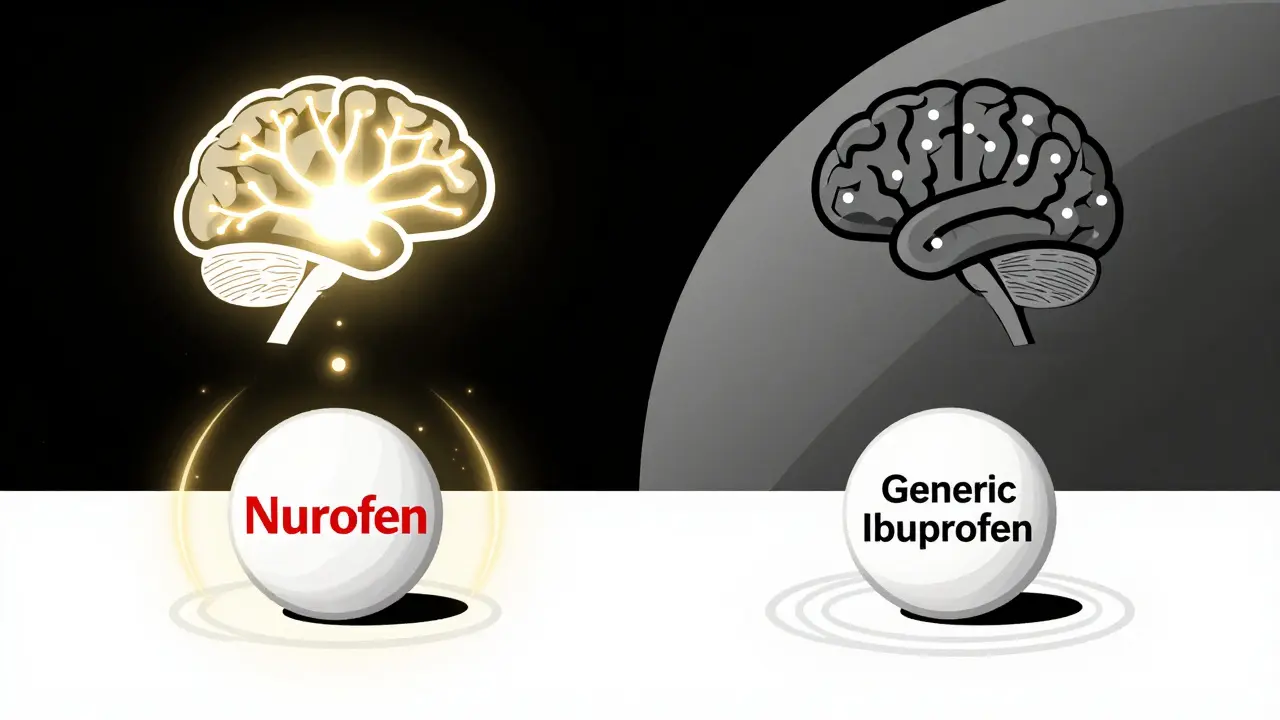
When you pick up a prescription, do you ever wonder why some people say their generic medication just doesn’t work as well as the brand name? It’s not just in their head. In fact, science shows it’s in their brain-and it’s changing how their body responds to the drug, even when the chemistry is identical.
Same pill, different results
Take ibuprofen. The active ingredient in Nurofen, Advil, and every generic version on the shelf is exactly the same: 200 mg of ibuprofen. But in a 2016 study, people who were given a sugar pill labeled as "Nurofen" reported pain relief just as strong as those who got real ibuprofen. Those who got the exact same sugar pill labeled "Generic Ibuprofen"? Their pain barely improved. The pills were identical. The only difference? The label. This isn’t a fluke. It’s the placebo effect in action-and it’s stronger than most people realize. When you believe a medicine will work, your brain releases natural painkillers like endorphins. It lowers stress hormones. It changes how your nervous system processes discomfort. That’s real biology. And when you think you’re taking a cheap, unfamiliar generic, your brain doesn’t trigger the same response.Branding isn’t just marketing-it’s medicine
The power of branding shows up in surprising ways. In one experiment, researchers gave people identical creams. One group was told it was a premium, expensive product. The other was told it was a low-cost generic. Both creams were inert-no active ingredients at all. But the people who thought they were using the expensive cream reported twice as much pain. Brain scans confirmed it: their pain-processing regions lit up more. Even their spinal cords showed stronger pain signals. That’s not imagination. It’s measurable. The same thing happens with pills. Brand-name labels activate areas of the brain linked to expectation and reward. Generic labels? Not so much. In fact, studies show brand-name labeling can boost the placebo effect by 30-40% in pain relief compared to generic labeling. For someone with chronic headaches, back pain, or arthritis, that difference can mean the difference between getting through the day and staying in bed.The dark side: when belief backfires
It’s not just about expecting relief. Sometimes, expecting harm makes it happen. That’s called the nocebo effect. In statin trials, patients were given dummy pills with no active drug. Yet 4-26% of them stopped taking them because they believed they were experiencing muscle pain, fatigue, or stomach issues. These weren’t side effects from the medicine-they were side effects from the fear of the medicine. One patient said, "I knew statins cause muscle problems, so I started noticing every little ache." And suddenly, every twinge became a symptom. Even the price tag can trigger this. When patients are told, "This generic costs less," they report more side effects-even if the pill is identical to the expensive version. Mentioning price doesn’t just affect perception; it rewires how the body feels pain and discomfort.Why do some people respond more than others?
Not everyone is equally affected. About 30% of people are highly suggestible-they’re more likely to feel stronger placebo or nocebo effects. Personality, past experiences, cultural beliefs, and even how much trust they have in their doctor play a role. Someone who’s had bad experiences with generics before is more likely to expect failure. Someone who’s been told "generics are just as good" by a trusted provider is more likely to believe it-and respond better. It’s not about intelligence or gullibility. It’s about how your brain interprets cues. A red pill might feel "stronger" than a white one. A large pill might feel "more potent." A bottle with a sleek design might feel "more professional." These tiny details shape your expectations-and your outcomes.
What does this mean for real patients?
In the U.S., 90% of prescriptions are filled with generics. They’re safe, effective, and save billions every year. But perception gaps are costing real health. Studies show patients are 27% more likely to quit taking a generic antidepressant within the first month compared to the brand-name version-even though blood tests confirm identical drug levels. That’s not because the generic doesn’t work. It’s because the patient doesn’t believe it will. The consequences add up. Poor adherence means more hospital visits, more flare-ups, more complications. Researchers estimate that negative perceptions of generics cost the U.S. healthcare system $1.2-$1.8 billion annually in avoidable care.How doctors and pharmacists can help
The good news? This isn’t hopeless. Small changes in how we talk about generics can make a big difference. One study found that if a doctor spends just 2-3 extra minutes explaining that generics are required by law to have the same active ingredient, same dosage, and same effectiveness as the brand, patient adherence jumps by 18-22%. That’s like adding a free treatment with no cost. Here’s what works:- Don’t say "just a generic." Say "this is the exact same medicine as [Brand Name], just without the marketing costs."
- Use FDA-approved language: "This medication is FDA-approved as an exact equivalent to [Brand Name]."
- Don’t mention price unless asked. If you do, pair it with reassurance: "It’s cheaper because we’re not paying for ads, not because it’s weaker."
- Consider packaging. Some newer generics now use clean, trusted color schemes (like blue and white) that signal reliability without being misleading.
Why generics still work-when you believe in them
There are plenty of people who take generics without issue. In fact, many report better outcomes once they understand the science. One Reddit user, a pharmacy tech, shared that when he explains to patients that generics must pass the same strict tests as brand-name drugs, many of them start feeling better. It’s not magic. It’s education. When people know the truth-that generics are held to the same standards, made in the same facilities, and monitored by the same agencies-they stop fearing them. And here’s the kicker: a 2023 study from Oxford found that giving patients a short video explaining how placebo effects work actually made generics more effective. Patients who watched it reported 28% better symptom relief than those who didn’t. Understanding the mechanism didn’t weaken the effect-it strengthened it.
The future: designing trust into medicine
Pharmaceutical companies are starting to pay attention. Teva’s "Advil Migraine" is a generic ibuprofen with a branded name and fancy packaging. It’s not better medicine. But it’s better perceived-and it’s capturing 17% of the migraine OTC market. Regulators are stepping in too. The FDA now advises doctors to avoid phrases like "it’s just a generic." The European Medicines Agency has standardized generic packaging across the EU to reduce confusion. The goal isn’t to trick people. It’s to align perception with reality. Because when you believe a treatment works, your body helps it work. And for millions of people on generics, that belief is the missing piece.What you can do
If you’re taking a generic and feel it’s not working:- Ask your doctor or pharmacist: "Is this the same as the brand name?"
- Check the FDA’s website for generic equivalence listings.
- Don’t assume it’s the drug-it might be your expectations.
- Give it time. Some effects take weeks to build, especially with antidepressants or blood pressure meds.
- Try reframing: "This is the same medicine, just less expensive."
- Use clear, confident language when prescribing generics.
- Address concerns before they become doubts.
- Don’t apologize for prescribing a generic. Be proud of it.
Final thought
Medicine isn’t just chemistry. It’s psychology. It’s trust. It’s belief. The placebo effect isn’t a flaw in treatment-it’s part of how healing works. And when we ignore the power of perception, we’re leaving real results on the table. Generics aren’t second-rate. They’re science-made-smart. The only thing holding them back? The stories we tell ourselves about them.Do generic drugs have the same active ingredients as brand-name drugs?
Yes. By law, generic drugs must contain the same active ingredient, in the same strength, and in the same form as the brand-name version. The FDA requires generics to be bioequivalent-meaning they deliver the same amount of medicine into your bloodstream within 8-13% of the brand-name drug. That’s well within the range considered safe and effective.
Can placebos really work as well as real medication?
In some cases, yes-for conditions where symptoms are heavily influenced by perception, like pain, anxiety, depression, and fatigue. Studies show placebo pills labeled as brand-name drugs can produce pain relief equal to real ibuprofen. That doesn’t mean the drug isn’t working-it means your brain’s response is a powerful part of the healing process.
Why do some people feel worse on generics?
It’s usually not the drug. It’s the belief. If someone expects a generic to be weaker or less safe, their brain can trigger physical symptoms-like headaches, nausea, or fatigue-through the nocebo effect. This is especially common when patients are told the drug is "cheaper" or "not the same." The body responds to the message, not just the molecule.
Is it true that expensive placebos cause more pain?
Yes. In controlled studies, people given identical placebo creams reported more pain when told the cream was expensive. Brain scans showed increased activity in pain-processing areas, and even spinal cord signals confirmed greater pain response. This proves that expectations can alter physical sensation-not just perception.
Should I avoid generics to get better results?
No. Generics are just as effective as brand-name drugs for nearly all conditions. The difference isn’t in the pill-it’s in your mind. If you’re concerned, talk to your doctor. Ask for reassurance, not a brand. Many patients feel better once they understand the science behind generics.
Can education improve how well generics work?
Absolutely. A 2023 Oxford study found that patients who watched a short video explaining how placebo effects work reported 28% better symptom relief from generics. Understanding that your expectations influence your outcomes helps you harness that power-instead of letting fear control it.

Patrick Merrell
January 26, 2026 AT 20:07This is why I refuse to take generics. I don't care what the FDA says. My body knows the difference. Brand names cost more because they work better. It's not placebo-it's physics. You can't trick biology with a different label.
SWAPNIL SIDAM
January 28, 2026 AT 01:51Bro, I used to think same thing. Then my uncle got diabetes. He switched to generic metformin. Saved him $800 a year. Same result. No drama. Just cheaper science. Trust the process.
Nicholas Miter
January 28, 2026 AT 18:47Actually, this makes a lot of sense. I used to get migraines and swore brand-name Excedrin was the only thing that worked. Switched to generic and it felt like nothing. Then I read this stuff and started telling myself, 'this is the same.' Within a week, it worked just as well. Mind is wild.
Suresh Kumar Govindan
January 29, 2026 AT 16:23The pharmaceutical-industrial complex has engineered this psychological dependency to maintain profit margins. This is not medicine-it is behavioral conditioning disguised as healthcare. The FDA is complicit. The entire system is a fraud.
Aishah Bango
January 30, 2026 AT 17:31I used to hate generics because I thought they were 'cheap junk.' Then I started reading the studies. Turns out, my brain was the problem. Now I take them without a second thought. And yeah-I feel better. Not because they're different. Because I stopped doubting them.
Angie Thompson
January 31, 2026 AT 21:05OMG YES!! I was skeptical too, but after my doc showed me the FDA charts and I watched that Oxford video? I felt like I’d been brainwashed by ads my whole life 😭💊 Now I tell everyone: it’s not the pill, it’s the story you tell yourself. And guess what? I’m saving $$$ AND feeling great!
Geoff Miskinis
February 1, 2026 AT 08:27How quaint. You believe a label alters neurochemistry? This is the kind of pseudoscience that gives psychology a bad name. The placebo effect is real, but to attribute therapeutic efficacy to branding is to ignore pharmacokinetics entirely. You're not treating illness-you're performing ritual.
Sally Dalton
February 3, 2026 AT 04:59so i just had this moment where i realized i was avoiding my generic blood pressure med because i thought it was 'weaker'... and then i read this and i felt so dumb 😅 i started taking it again and my numbers are actually better now. thanks for this. really needed to hear it.
Betty Bomber
February 3, 2026 AT 19:12I’ve been a pharmacy tech for 12 years. I’ve seen people cry because they were switched to generics. Then they’d come back two weeks later saying, 'I don’t know what changed, but I feel way better.' Same pill. Different story.
Mohammed Rizvi
February 5, 2026 AT 18:18Let me guess… you’re the kind of person who thinks a $12 generic is 'bad' because it doesn’t come in a bottle with a gold cap and a 10-page insert. Meanwhile, your cousin in Mumbai takes the same generic and runs marathons. Wake up.
eric fert
February 7, 2026 AT 01:18Okay, but let’s be real here. If the placebo effect is so powerful, why aren’t we just giving people placebo pills and calling it a day? Why do we even need drugs? Why not just hand out branded candy and call it medicine? This whole thing is a slippery slope. If your brain can make a sugar pill work, then why not just tell people to 'think happy thoughts' for cancer? Where do we draw the line? And don’t say 'it’s not that extreme'-because it is. This is how cults start. People believe so hard in something that it becomes real. But reality doesn’t care what you believe. And if we start letting perception dictate treatment, we’re one step away from homeopathy being covered by insurance. And don’t even get me started on the corporate manipulation angle. Big Pharma isn’t trying to help you-they’re trying to sell you the illusion that you’re getting something better. And we’re all just complicit.
Ryan W
February 8, 2026 AT 20:30