Oral Diabetes Medications Compared: Metformin, Sulfonylureas, and GLP-1 Agonists
 Jan, 30 2026
Jan, 30 2026
When you're managing type 2 diabetes, choosing the right medication isn't just about lowering blood sugar-it's about fitting your life, your body, and your risks. Three main oral (or mostly oral) drugs dominate the landscape: metformin, sulfonylureas, and GLP-1 receptor agonists. Each works differently, has different side effects, and affects your long-term health in unique ways.
Metformin: The Longtime Standard
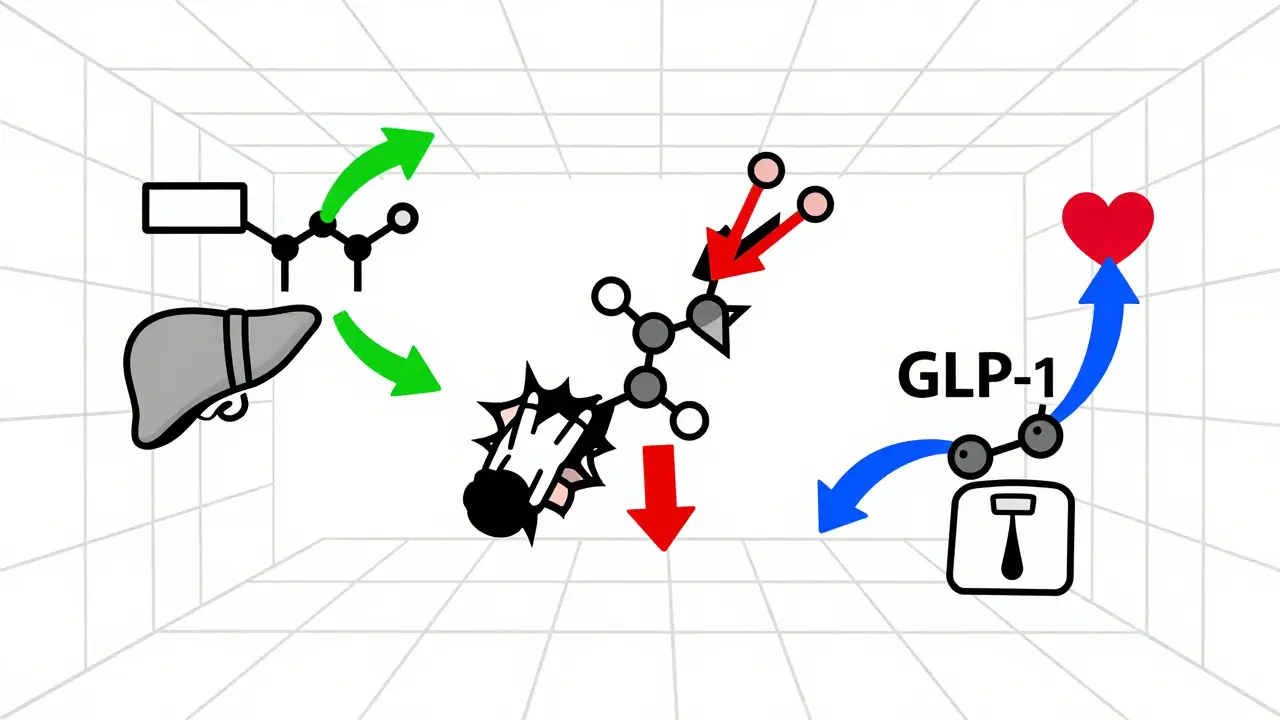
Metformin has been the go-to first-line treatment for type 2 diabetes since the mid-1990s, and for good reason. It’s cheap, safe for most people, and doesn’t cause weight gain or low blood sugar when used alone. It works by reducing how much sugar your liver makes and helping your muscles use insulin better. Most people take it twice a day with meals to cut down on stomach upset.On average, metformin lowers HbA1c by 1% to 2%. That’s solid-but not flashy. About 20% to 30% of people get nausea, diarrhea, or gas when they start. Many of these side effects fade after a few weeks, especially if you switch to the extended-release version. Some people never tolerate it, no matter the dose or brand. One Reddit user wrote, “I’ve tried every form of metformin. The diarrhea never stops. I had to stop.”
Metformin is also weight neutral or can help you lose a few pounds-around 2 to 3 kg on average. It’s been linked to lower heart disease risk and even some protection against certain cancers, though those benefits are still being studied. The biggest red flag? Lactic acidosis, a rare but serious condition. That’s why doctors check your kidney function before prescribing it. If your eGFR drops below 30, you shouldn’t take it.
Sulfonylureas: Old School, High Risk
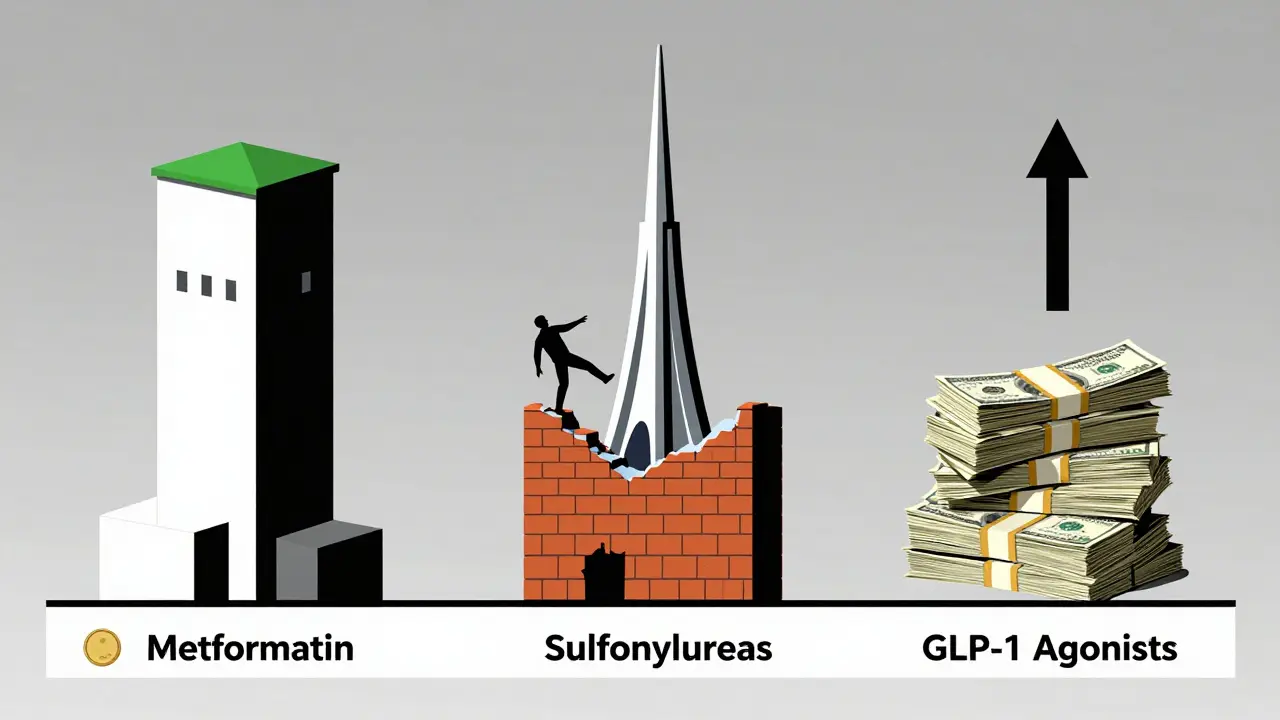
Sulfonylureas like glipizide and glimepiride have been around since the 1950s. They force your pancreas to pump out more insulin, which lowers blood sugar fast. That’s why they work well in the short term. But that same mechanism is also their biggest flaw.Sulfonylureas lower HbA1c by about 1% to 1.5%, similar to metformin. But here’s the catch: they cause low blood sugar-often. Up to 30% of people on these drugs have mild to moderate hypoglycemia each year. About 2% to 4% have episodes bad enough to need emergency care. One patient on HealthUnlocked shared: “I had four ER visits in three years because my blood sugar crashed. I didn’t even feel it coming.”
They also cause weight gain-typically 2 to 4 kg. That’s the opposite of what most people with type 2 diabetes need. And unlike metformin or GLP-1 agonists, they don’t offer any heart protection. In fact, some studies suggest they might slightly increase heart risk compared to other options.
Doctors still prescribe them because they’re cheap-$10 to $30 a month-and effective. But they’re being used less often. The American College of Physicians says sulfonylureas increase hypoglycemia risk more than any other diabetes drug. If you’re older, have kidney issues, or skip meals often, they’re usually not the best choice.
GLP-1 Agonists: The New Powerhouse
GLP-1 receptor agonists changed the game. Originally injectable drugs like liraglutide (Victoza) and semaglutide (Ozempic), they now include an oral version: semaglutide (Rybelsus). These drugs mimic a natural hormone that tells your pancreas to release insulin only when blood sugar is high-so they rarely cause low blood sugar unless mixed with sulfonylureas or insulin.They lower HbA1c by 0.8% to 1.5%, slightly less than metformin on paper, but they do something no other oral diabetes drug can: they help you lose weight. Most people lose 3 to 6 kg. Some lose much more. One user on the ADA forums said, “I lost 18 pounds in three months. My A1C dropped from 7.8 to 6.2. I didn’t change my diet.”
They also protect your heart. The LEADER trial showed liraglutide reduced major heart events by 13%. Semaglutide and dulaglutide showed similar results. They’re now recommended as second-line therapy for people with heart disease, kidney disease, or high heart risk-even if their A1C is already under control.
The downside? Stomach issues. Nausea, vomiting, and diarrhea affect 20% to 40% of users, especially when starting or increasing the dose. Most people adjust after 4 to 12 weeks. Slow dose escalation helps. And while the oral version (Rybelsus) avoids needles, it still causes nausea and must be taken on an empty stomach with just a sip of water-no food, no other drinks-for at least 30 minutes after.
Cost is a major barrier. Without insurance, these drugs cost $700 to $900 a month. With insurance, copays can still be $50 to $200. That’s why many people can’t access them, even though they’re more effective and safer long-term.

How They Stack Up
| Feature | Metformin | Sulfonylureas | GLP-1 Agonists |
|---|---|---|---|
| Average HbA1c reduction | 1.0%-2.0% | 1.0%-1.5% | 0.8%-1.5% |
| Weight effect | Neutral or slight loss (2-3 kg) | Gain (2-4 kg) | Loss (3-6 kg) |
| Hypoglycemia risk | Very low (alone) | High (15-30% yearly) | Low (unless combined) |
| Cardiovascular benefit | Moderate | Neutral or slightly negative | Strong (13%+ reduction in events) |
| Common side effects | Diarrhea, nausea (20-30%) | Low blood sugar, weight gain | Nausea, vomiting (20-40%) |
| Cost (monthly, generic) | $4-$10 | $10-$30 | $700-$900 (without insurance) |
| Administration | Oral, 1-2x/day | Oral, 1-2x/day | Oral or injectable, daily or weekly |
Who Gets What-and Why
If you’re just starting diabetes meds, metformin is still the best first choice for most people. It’s safe, affordable, and doesn’t cause low blood sugar. But if you can’t tolerate it-or if you’re overweight, have heart disease, or want to lose weight-GLP-1 agonists are the next best thing.Sulfonylureas? They’re fading out. They’re only really considered if cost is the only barrier and other options aren’t available. Even then, doctors often avoid them in older adults, people with kidney problems, or those who don’t eat regularly.
Recent guidelines from the American Diabetes Association now say GLP-1 agonists should be considered early-even as a first choice-for patients with heart failure, chronic kidney disease, or very high heart risk. That’s a big shift. Ten years ago, that would’ve been unthinkable.
Real-Life Trade-Offs
There’s no perfect drug. It’s about balancing benefits and burdens.If you’re on a tight budget and your A1C is only slightly high, metformin might be enough. But if you’re struggling with weight, have heart disease, or hate the idea of another needle, the oral GLP-1 agonist (Rybelsus) could be worth the cost. It’s not just about sugar numbers-it’s about your energy, your heart, your future.
One doctor told a patient: “Metformin keeps you alive. GLP-1 agonists help you live better.” That’s the difference.
What’s Next?
The future of diabetes meds is moving fast. New drugs like retatrutide-triple agonists that target GLP-1, GIP, and glucagon-are showing HbA1c drops of over 3% and weight loss of nearly 25% in trials. These could be game-changers.Meanwhile, biosimilars of GLP-1 drugs are coming, which could cut prices by 70% or more in the next few years. Experts predict that within five years, GLP-1 agonists will be first-line for most people-not because they’re better at lowering sugar, but because they protect your whole body.
For now, your choice depends on your health, your budget, and your goals. Talk to your doctor about what matters most: just controlling blood sugar? Or living longer, healthier, and lighter?”
Is metformin still the best first choice for type 2 diabetes?
Yes, for most people. Metformin is still the first-line recommendation by the American Diabetes Association because it’s effective, safe, affordable, and doesn’t cause low blood sugar or weight gain. But if you can’t tolerate it or have heart disease, kidney disease, or obesity, GLP-1 agonists are now strongly recommended as an alternative-even as a first option in some cases.
Why are GLP-1 agonists so expensive?
GLP-1 agonists are biologic drugs, which are complex and costly to manufacture. They’re also relatively new, and brand-name versions like Ozempic and Rybelsus are still under patent protection. Without insurance, they can cost $700-$900 per month. Biosimilars are in development and could drop prices significantly within the next few years.
Can I take sulfonylureas if I’m worried about weight gain?
Probably not. Sulfonylureas consistently cause weight gain-typically 2 to 4 kg-because they force your body to produce more insulin, which promotes fat storage. If weight is a concern, metformin or GLP-1 agonists are better options. Metformin is weight neutral or may help you lose a little, while GLP-1 agonists lead to significant weight loss.
Do GLP-1 agonists cause low blood sugar?
Not when taken alone. GLP-1 agonists only stimulate insulin release when blood sugar is high, so they rarely cause hypoglycemia on their own. But if you combine them with sulfonylureas or insulin, your risk of low blood sugar increases significantly. Always tell your doctor about all your medications.
Is the oral version of semaglutide (Rybelsus) as effective as the injection?
Yes, but slightly less so. Rybelsus lowers HbA1c by about 1.0% to 1.3%, while injectable semaglutide (Ozempic) lowers it by 1.3% to 1.8%. The oral version requires strict dosing rules: taken on an empty stomach with just a sip of water, 30 minutes before food or drink. Adherence is lower than with injections, but many people prefer it for convenience.
What should I do if I can’t afford GLP-1 agonists?
Talk to your doctor about alternatives. Metformin remains the most affordable option. Some manufacturers offer patient assistance programs that can reduce copays to $0 for eligible patients. Also, check if your insurance covers generic sulfonylureas or SGLT2 inhibitors like Jardiance, which have heart and kidney benefits too. Never stop your meds because of cost-ask for help first.

Sazzy De
January 31, 2026 AT 03:45Kimberly Reker
January 31, 2026 AT 12:58Mike Rose
January 31, 2026 AT 13:37Russ Kelemen
February 1, 2026 AT 11:23Diksha Srivastava
February 2, 2026 AT 21:51Sidhanth SY
February 4, 2026 AT 03:08Adarsh Uttral
February 5, 2026 AT 02:35Beth Cooper
February 5, 2026 AT 22:56Donna Fleetwood
February 6, 2026 AT 07:36kate jones
February 6, 2026 AT 23:05Marc Bains
February 8, 2026 AT 04:08Melissa Cogswell
February 8, 2026 AT 14:20Beth Beltway
February 9, 2026 AT 20:55Kelly Weinhold
February 11, 2026 AT 08:56KATHRYN JOHNSON
February 12, 2026 AT 16:03