Next-Generation GLP-1 Agents: Safety Profiles and Side Effects
 Feb, 11 2026
Feb, 11 2026
GLP-1 Side Effect Risk Calculator
How Your Individual Factors Affect Side Effect Risk
Based on clinical data from Phase II/III trials of next-generation GLP-1 agents (retatrutide, orforglipron, VK2735)
Nausea Risk
Vomiting Risk
Muscle Loss Risk
Important Safety Note
Based on 2025 clinical data: Over 20% weight loss increases risk of muscle and bone density loss. Always consult your healthcare provider before starting treatment.
Personalized Recommendations
When you hear about GLP-1 agonists, you might think of Ozempic or Wegovy - the injectables that made headlines for helping people lose significant weight. But those are just the beginning. By 2026, a new wave of next-generation GLP-1 agents is hitting the market, promising even better results - and with them, new questions about safety. These aren’t just upgraded versions of old drugs. They’re fundamentally different: some are oral, others hit three hormone receptors at once, and a few are designed to keep working long after you stop taking them. But with greater power comes greater complexity. What do these new drugs actually do to your body? And what are the real risks you won’t hear about in ads?
What Makes a GLP-1 Agent "Next-Generation"?
First-generation GLP-1 receptor agonists like liraglutide and exenatide worked by mimicking the natural hormone GLP-1. That hormone tells your pancreas to release insulin when you eat, slows your stomach emptying, and signals your brain that you’re full. The result? Better blood sugar control and modest weight loss - usually 5-10% of body weight.
Next-generation agents go further. Retatrutide is a triple agonist - it activates not just GLP-1, but also GIP and glucagon receptors. This three-pronged approach led to an average weight loss of 17.5% after just 24 weeks in Phase II trials, and up to 24.2% after 48 weeks at the highest dose. Retatrutide is a next-generation triple GLP-1/GIP/glucagon receptor agonist under Phase III development by Eli Lilly, with results expected in late 2025/2026.
Orforglipron is different again. It’s the first oral GLP-1 agonist to show serious weight loss potential. In trials, patients lost 15-20% of their body weight over a year. That’s comparable to injectables - but taken as a pill. It also lowered systolic blood pressure by an average of 4.2 mm Hg. Orforglipron is an oral GLP-1 receptor agonist developed by Merck, with Phase III trials ongoing as of 2025.
And then there’s VK2735, a dual GLP-1/GIP agonist similar to tirzepatide. In Phase 2 trials, it delivered nearly 15% weight loss in just 13 weeks. Even more surprising? A Phase 1 oral version showed 5% weight loss in just one month. That’s faster than most injectables.
These aren’t just about weight. They’re designed to reset metabolism. By targeting multiple hormone pathways, they’re moving beyond diabetes and obesity into areas like fatty liver disease, heart failure, and even neurodegenerative conditions. But that also means we’re entering uncharted territory.
Common Side Effects: The Gastrointestinal Reality
If you’ve ever tried semaglutide or liraglutide, you know the drill: nausea, vomiting, diarrhea, constipation. These aren’t rare - they affect 30-50% of users. And guess what? The newer drugs don’t fix this.
A 2025 study by Wen et al. (PMID: 40685266) found that despite the theory that adding GIP or glucagon might reduce GI upset, the opposite happened. Patients on retatrutide and orforglipron reported nausea and vomiting at rates similar to older drugs. In fact, at maximum doses, GI side effects were just as common - sometimes worse.
Here’s what the data shows for next-gen agents:
- Nausea: 25-40% of users, especially during dose escalation
- Vomiting: 10-20%, peaks around week 4-8
- Diarrhea: 12-18%
- Constipation: 10-15%
What’s different now is the speed. With oral agents like orforglipron, side effects can hit harder and faster. One patient in a 2024 trial reported severe nausea within hours of taking the first dose - something rarely seen with injectables, which are titrated slowly.
Here’s the good news: 70-80% of people find these symptoms fade within 4-8 weeks. The body adapts. But that doesn’t help if you’re one of the 5-10% who can’t tolerate it. Discontinuation rates climb sharply at higher doses - especially with agents like retatrutide, where the 12mg dose is where the real weight loss kicks in.
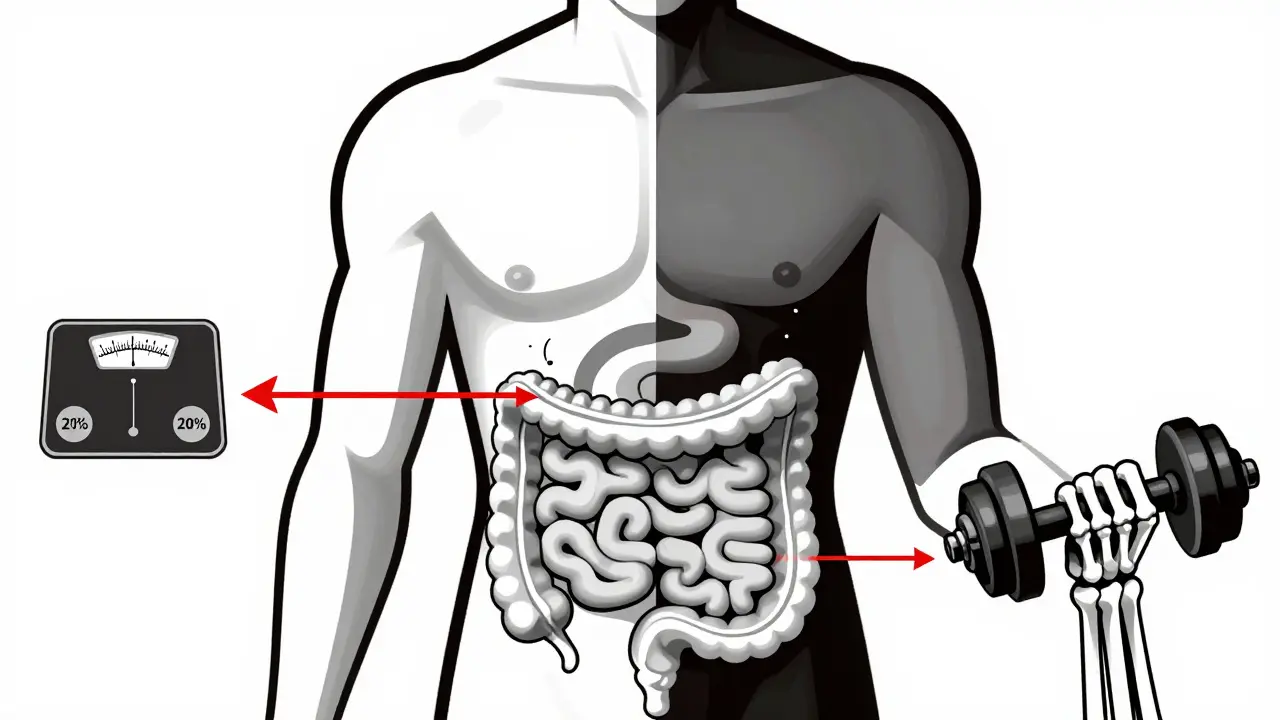
The Hidden Risks: Muscle, Bone, and Beyond
Most people focus on nausea. But the real concerns are quieter - and more dangerous.
Dr. Daniel J. Drucker, a leading researcher at the University of Toronto, warned in his 2025 Nature Reviews article that rapid, massive weight loss - think 20% or more - doesn’t just burn fat. It can also burn muscle. In clinical trials, some patients lost up to 30% of their lean body mass alongside fat. That’s not just about looking leaner. It’s about strength, mobility, and long-term metabolic health.
That’s why experts now recommend combining these drugs with resistance training and adequate protein intake. Without it, you might lose weight - but also lose the ability to walk, climb stairs, or recover from injury.
Another silent risk? Bone density. A 2025 analysis from the Obesity Care Clinic noted that patients losing over 20% of body weight showed measurable declines in hip and spine bone mineral density. The effect was strongest in postmenopausal women and older adults. Long-term studies are still ongoing, but the message is clear: if you’re on one of these drugs for years, you need bone scans.
Pancreatitis remains a theoretical risk. The American Gastroenterological Association’s 2022 guidelines still list it as a concern, though actual cases in trials are rare. Still, if you have a history of pancreatitis, these drugs are not recommended.
And then there’s the issue of long-term use. We have 5-10 years of data on semaglutide. We have less than 2 years on retatrutide and orforglipron. What happens after 10 years? 20 years? We don’t know. That’s why Dr. Elena Grunvald, lead author of the AGA guidelines, says we’re still in the early innings.
The Compounded Drug Danger
If you’ve seen ads for "semaglutide" from online pharmacies offering $50 vials, you’re not alone. But here’s the truth: those aren’t the same as the FDA-approved versions.
The University of Illinois at Chicago’s Digital Pharmacy issued a stark warning in August 2025: compounded GLP-1 products have 3-5 times higher rates of adverse events. Why? Because they’re not regulated. Doses vary. Purity isn’t guaranteed. Some batches contain too much active ingredient - leading to severe nausea, low blood sugar, or even hospitalization. Others contain too little, making them useless.
One case study from a Chicago hospital in early 2025 involved a patient who developed acute kidney injury after taking a compounded "GLP-1" product that turned out to contain an unapproved stimulant. The pharmacy had no quality control. No batch testing. No traceability.
There’s no such thing as a "generic" GLP-1 agonist yet. These drugs are too complex to copy. If it’s not made by Novo Nordisk, Eli Lilly, or Merck - it’s a gamble.
What Should You Do?
These drugs aren’t magic. They’re powerful tools - and like any tool, they need careful handling.
- If you’re considering one, start with an FDA-approved version. Don’t rush into oral or triple agonists unless your doctor has reviewed your full health history.
- Ask about dose titration. Slow starts reduce side effects. Don’t skip the first few weeks.
- Track your muscle mass and bone density. Ask your doctor for a DEXA scan before starting and again after 12 months.
- Never use compounded versions. If your insurance won’t cover the brand-name drug, talk to your provider about alternatives - not shortcuts.
- Combine with strength training and protein. Aim for 1.6-2.2 grams of protein per kg of body weight daily.
The future of GLP-1 therapy is personalized. New agents are being designed to match metabolic phenotypes - so someone with insulin resistance might get one combo, while someone with slow gastric emptying gets another. But that future only works if we understand the risks - not just the rewards.
What’s Coming Next?
By late 2026, we should have full Phase III data on retatrutide and orforglipron. Both are expected to seek FDA approval for obesity treatment. But the real story isn’t just weight loss. It’s what happens after.
Eli Lilly’s trials now include detailed monitoring of muscle loss, kidney function, and cardiovascular outcomes. Viking Therapeutics is testing whether VK2735’s oral form causes fewer GI issues than injectables. And researchers are starting trials for GLP-1 agents in Alzheimer’s, Parkinson’s, and even depression.
But here’s the bottom line: the safest GLP-1 agent is the one you can tolerate. The best one isn’t necessarily the one that loses the most weight - it’s the one that keeps you healthy for the long haul.
Are next-generation GLP-1 agents safer than older ones?
No - not in terms of side effects. While newer agents like retatrutide and orforglipron offer better weight loss, their most common side effects - nausea, vomiting, and diarrhea - are just as frequent, if not worse, than older drugs like semaglutide. The difference lies in potency and delivery method, not safety. The long-term safety of losing over 20% of body weight is still unknown.
Can I take oral GLP-1 agonists like orforglipron instead of injections?
Yes - but only if approved by your doctor and you’re prescribed an FDA-approved version. Orforglipron is one of the first oral GLP-1 agonists to show strong results, with weight loss comparable to injectables. However, it’s not yet FDA-approved as of early 2026. Clinical trials are ongoing, and it may become available by late 2026. Never substitute with compounded versions.
Do these drugs cause muscle loss?
Yes - especially at high doses and with rapid weight loss. Studies show patients on agents like retatrutide can lose up to 30% of lean muscle mass alongside fat. This is why experts now recommend combining these drugs with resistance training and high protein intake (1.6-2.2 g/kg daily). Without these measures, long-term strength and mobility can be affected.
Are compounded GLP-1 drugs safe?
No. Compounded GLP-1 products are not FDA-approved and vary widely in potency and purity. The University of Illinois at Chicago reported 3-5 times more adverse events from compounded versions compared to branded drugs. Risks include overdose, contamination, and serious reactions like kidney injury. Always use only FDA-approved medications from licensed pharmacies.
How long do side effects last?
For most people, gastrointestinal side effects like nausea and vomiting improve within 4 to 8 weeks as the body adjusts. However, at maximum doses - especially with newer agents - side effects can persist longer. If symptoms don’t improve after 12 weeks, your doctor may need to lower your dose or switch therapies.
Is there a risk of pancreatitis with next-gen GLP-1 agents?
The risk is low but not zero. The American Gastroenterological Association still lists pancreatitis as a theoretical concern. In clinical trials, cases have been rare - fewer than 1 in 1,000 patients. But if you have a history of pancreatitis, these drugs are generally avoided. Always report persistent abdominal pain to your doctor immediately.
Will these drugs be covered by insurance in 2026?
Coverage is improving but still inconsistent. As of 2025, most major insurers cover semaglutide and tirzepatide for obesity, but newer agents like retatrutide and orforglipron may not be covered until after FDA approval - likely late 2026. Some plans require prior authorization or proof of failed diet and exercise attempts. Always check with your insurer before starting.

Gloria Ricky
February 12, 2026 AT 09:54Just started retatrutide last month and wow. Nausea hit me like a truck week 1, but by week 4? Gone. I’m losing weight like I’m in a sci-fi movie. Protein intake and lifting 3x a week saved my muscles. Seriously, don’t skip the weights. Also, no compounding crap - I paid the insurance copay and it was worth every penny.
Sonja Stoces
February 12, 2026 AT 20:50LMAO you all act like these drugs are magic. 🤡 They’re just fancy appetite suppressants with a 20% chance of puking your guts out. And muscle loss? Please. You think your ‘fitness routine’ is gonna save you? Nah. You’re just buying time before your metabolism crashes harder than a Bitcoin investor in 2022. 💩
Annie Joyce
February 13, 2026 AT 00:57Okay, real talk - I’m a nurse who’s seen 17 patients on these next-gen GLP-1s. The GI stuff? Brutal at first, but 80% of folks adapt. The bone density drop? Yeah, it’s real. I push DEXA scans like it’s my job (because it is). And PLEASE stop buying ‘GLP-1’ off Telegram. One patient ended up in the ER with a potassium crash because their ‘oral pill’ had 3x the dose. It’s not a supplement. It’s a pharmaceutical. Treat it like it’s your grandma’s heart med.
Luke Trouten
February 13, 2026 AT 07:35There’s a deeper philosophical question here: are we treating disease, or optimizing human biology beyond its evolutionary design? These drugs don’t just alter metabolism - they redefine what ‘normal’ weight means. If we’re engineering weight loss at 24%, are we also engineering unintended consequences into our physiology? The data is promising, but the wisdom isn’t there yet. We’re rushing toward a future we don’t fully understand.
Kristin Jarecki
February 14, 2026 AT 12:41Thank you for this comprehensive and evidence-based overview. I would like to emphasize the importance of multidisciplinary care when initiating these therapies. Endocrinology, physical therapy, nutrition, and bone health monitoring should be integrated into the treatment plan from day one. Patient education is not optional - it is foundational to long-term safety and efficacy. I urge all clinicians to adopt standardized protocols for baseline and follow-up assessments.
Jonathan Noe
February 14, 2026 AT 14:48Did you know that VK2735’s oral version works faster because it bypasses the liver’s first-pass metabolism? That’s why you see 5% loss in a month. Also, the GIP component doesn’t just help with weight - it boosts insulin sensitivity in skeletal muscle. And no, you can’t just ‘take a break’ from it - the half-life is like 14 days. So if you stop, you’re not just gaining weight back - you’re resetting your hunger hormones. This isn’t dieting. This is metabolic reprogramming. And yeah, the nausea? That’s your gut screaming because it’s been trained to expect carbs for 50,000 years. Now it’s being told to shut up. Give it time.
Suzette Smith
February 16, 2026 AT 08:49Wait, so you’re telling me the drugs that make you lose 24% of your body weight are ALSO the ones that make you lose muscle and bone? Hmm. So… are we just turning people into skeletons with better blood sugar? 🤔
andres az
February 18, 2026 AT 04:18They’re not ‘next-gen’ - they’re lab-made mind control. The FDA’s approval process is a joke. Big Pharma is pushing these because they know once you’re on it, you’re hooked - and they’ll charge $1,200/month. Bone scans? Muscle loss? That’s just collateral damage. Meanwhile, the real solution - intermittent fasting, whole foods, sleep - is ignored because it doesn’t have a patent. Wake up. This is a cash grab disguised as medicine.