Mouth Sores from Medications: How to Prevent and Care for Them
 Nov, 23 2025
Nov, 23 2025
Mouth Sores Risk Calculator
This tool helps estimate your risk of developing mouth sores (oral mucositis) during cancer treatment based on your treatment type, dental health, and prevention habits. Risk is calculated from factors mentioned in the article.
When you’re undergoing cancer treatment, the last thing you want is to be in constant pain just from talking or eating. Yet for many people on chemotherapy or radiation, painful mouth sores and ulcers - known medically as oral mucositis - become a regular, crushing part of daily life. These aren’t just minor irritations. They’re open wounds in the lining of your mouth, throat, or tongue, caused directly by the drugs meant to save your life. The pain can be so severe that swallowing becomes impossible, leading to dehydration, weight loss, and even hospitalization. The good news? You don’t have to just suffer through it. There are proven, science-backed ways to prevent these sores before they start - and manage them effectively when they do.
Why Medications Cause Mouth Sores
Chemotherapy and radiation don’t just target cancer cells. They also attack any rapidly dividing cells in your body - including the ones that line your mouth. This damage triggers inflammation, breaks down the protective barrier of your oral tissue, and opens the door to painful ulcers. The severity varies: some people get mild redness, while others develop deep, bleeding sores that make eating or speaking unbearable. According to a 2022 NIH review, between 20% and 100% of cancer patients develop these sores, depending on the type and intensity of treatment. High-dose chemo for stem cell transplants, head and neck radiation, and drugs like 5-fluorouracil or melphalan carry the highest risk.
It’s not just about the drug itself. Factors like poor dental health, smoking, dehydration, and even the type of toothpaste you use can make things worse. Sodium lauryl sulfate (SLS), a common foaming agent in many toothpastes, strips away protective mucus and irritates already sensitive tissue. That’s why switching to an SLS-free toothpaste is one of the simplest, cheapest, and most effective steps you can take.
Prevention Is the Only Real Win
Once a mouth ulcer forms, treatment options are limited and often only ease pain - they don’t heal it faster. That’s why experts agree: prevention is the only strategy that truly works. The Multinational Association of Supportive Care in Cancer (MASCC) and International Society of Oral Oncology (ISOO) updated their guidelines in 2020 to make this crystal clear: focus on stopping sores before they start.
Here’s what works - backed by clinical trials and real patient outcomes.
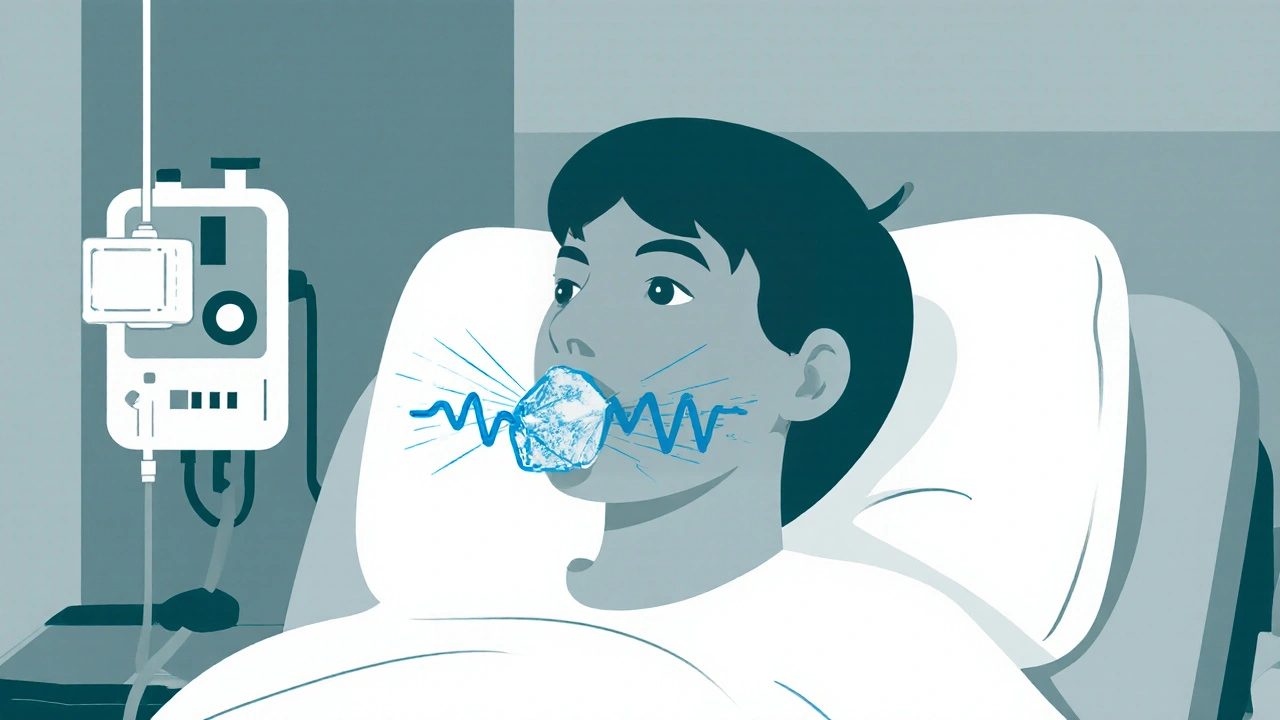
1. Cryotherapy: Ice Chips for Certain Chemotherapies
If you’re getting melphalan or 5-fluorouracil, sucking on ice chips is one of the most powerful tools you have. It’s simple, free, and effective. The cold narrows blood vessels in your mouth, reducing how much chemo reaches your oral tissues. Studies show this cuts the risk of severe ulcers by half.
But timing matters. You must start sucking on ice chips 5 minutes before your infusion begins and keep going for a full 30 minutes after. No breaks. No sipping - just continuous sucking. A 2021 MASCC study found that 87% adherence was needed to see real results. If you miss even a few minutes, the protection drops.
Some people hate it. The cold is intense. But 78% of patients on CancerCare’s forum reported it was "very or somewhat helpful." If you have cold sensitivity, try smaller chips or crushed ice. It’s still worth it.
2. Benzydamine Mouthwash: First-Line for Radiation
For patients getting radiation to the head or neck, benzydamine hydrochloride 0.15% mouthwash is the gold standard. It’s an anti-inflammatory that reduces swelling and pain right where it’s needed. A 2020 MASCC/ISOO review found it lowers the chance of severe mouth sores by 34%.
Use it 3-4 times a day, starting before treatment begins. Swish for 30 seconds, then spit. Don’t swallow. Use it 15 minutes before meals so food doesn’t wash it away. It stings at first - 68% of users report that - but 82% keep using it because the pain relief is real.
Cost? Around $15-$25 per course. That’s a fraction of what other options cost. It’s also not recommended if you’re allergic to aspirin or other NSAIDs.
3. Dental Checkup Before Treatment
Many people skip this. Don’t. A dental exam 2-4 weeks before starting chemo or radiation is critical. Your dentist can remove infected teeth, fix broken fillings, or treat gum disease - all things that can turn into major infections once your immune system is down. According to Roswell Park’s 2024 protocol, 78% of severe oral mucositis cases could be prevented with proper pre-treatment dental care.
Ask for a soft-bristle toothbrush (bristles under 0.008 inches) and fluoride toothpaste. Brush gently 2-3 times a day. Rinse after meals with a baking soda solution: 1 teaspoon in 8 ounces of water. It neutralizes acid and soothes irritation.
4. Avoid Chlorhexidine - It’s Overused
You’ve probably heard of chlorhexidine mouthwash. It’s common in hospitals and often prescribed. But here’s the truth: it only reduces risk by 15%, according to the 2022 NIH review. Worse, long-term use can stain your teeth and tongue brown. A 2020 patient survey in Oral Diseases found 28% of users had taste changes or a burning sensation.
Dr. Robert Worsham at MD Anderson calls over-reliance on chlorhexidine "false security." It’s not useless, but it shouldn’t be your main defense. Use it only if your care team specifically recommends it - and never as a substitute for proven methods like cryotherapy or benzydamine.
What to Use When Sores Happen
Even with prevention, sores can still appear. When they do, your goal is pain relief and keeping the area clean.
Gelclair: The Pain Reliever That Works
Gelclair is a mucoadhesive gel - meaning it sticks to your mouth like a protective film. It contains polyvinylpyrrolidone, sodium hyaluronate, and glycerin. It doesn’t heal ulcers, but it coats them and blocks pain signals. In a 2018 BMC Cancer study, it provided relief for up to 4 hours per application.
On Reddit’s r/cancer community, users gave it a 4.2/5 rating. But 33% said the slimy texture made talking or eating awkward. If you can tolerate it, it’s one of the best over-the-counter options.
Dexamethasone Mouthwash: For Severe Pain
For intense pain, some clinics prescribe dexamethasone 0.5mg/5mL mouthwash. Swish and spit 4 times a day. A 2024 protocol from Roswell Park showed it reduced pain scores by 37% on a 10-point scale. It’s a steroid, so it’s not for long-term use - only during flare-ups.
Glutamine: Mixed Results, But Worth Trying
Glutamine is an amino acid that some believe helps repair tissue. In a 2017 JAMA Oncology trial, 15g dissolved in water, swished and swallowed 4 times a day, cut the duration of ulcers by 43%. But later studies have been inconsistent. A 2022 meta-analysis found it only worked for head and neck cancer patients on radiation - not for chemo-only cases.
Still, many patients swear by it. On HealthUnlocked, 37% of positive reviews mention swishing for 2 full minutes before swallowing. It’s cheap, safe, and worth a try if other options aren’t enough.

What Doesn’t Work - And What Could Hurt You
Not everything you hear online helps. Some advice is dangerous.
Don’t use benzocaine products. The FDA warned in 2021 that benzocaine (found in Orajel and similar gels) can cause methemoglobinemia - a rare but life-threatening blood disorder - especially in children. Avoid all topical numbing agents unless your doctor prescribes them.
Don’t use systemic antibiotics to prevent sores. The American Society of Clinical Oncology updated its 2022 guidelines to strongly discourage this. A 2021 JAMA Internal Medicine study found routine antibiotics increased the risk of Clostridium difficile infection by 27% - a dangerous gut infection that can be deadly.
Don’t ignore dry mouth. Radiation often causes xerostomia (dry mouth), which makes sores worse. Use artificial saliva products like Biotene, or ask your doctor about pilocarpine tablets. Pilocarpine 5mg taken 3 times daily can increase saliva flow by 47% over baseline, according to a 2022 Oral Surgery study.
Real Talk: What Patients Actually Do
Looking at real patient experiences gives you the full picture.
- 61% of users on Smart Patients recommend using a children’s toothbrush - softer bristles mean less irritation.
- 54% of people on the Canker Sore subreddit say avoiding SLS toothpaste made a noticeable difference.
- 92% of uninsured patients couldn’t afford palifermin, a powerful drug that reduces severe ulcers from 63% to 20% in transplant patients - but costs $10,500 per course.
- Many patients combine methods: ice chips before chemo, benzydamine during radiation, Gelclair when ulcers flare.
The takeaway? There’s no single magic solution. But combining a few proven strategies - prevention first, pain relief second - makes a huge difference.

What’s Coming Next
Research is moving fast. In March 2024, results from a phase 3 trial showed GC4419 - a superoxide dismutase mimetic - reduced severe mucositis duration by 38% in head and neck cancer patients. Low-level laser therapy (LLLT) is also gaining traction: a 2023 JAMA Network Open study found it cut severe ulcers from 41% to 18% when used with specific settings (650nm wavelength, 40mW power).
Memorial Sloan Kettering has developed a risk prediction tool that uses 12 clinical factors to identify high-risk patients with 84% accuracy. Soon, care won’t be one-size-fits-all. It’ll be personalized - based on your treatment, genetics, and oral health history.
But for now, the tools you need are already here. You don’t need expensive drugs or experimental treatments. You need to act early, use what’s proven, and speak up if something isn’t working.
Frequently Asked Questions
Can mouth sores from chemo be prevented completely?
Not always, but you can reduce the risk by up to 80% with the right prevention plan. Using cryotherapy for melphalan or 5-FU, benzydamine for radiation, and a dental checkup before treatment are the most effective steps. Even then, some people still develop mild sores - but they’re usually less severe and heal faster.
Is Gelclair better than salt water rinses?
Gelclair provides longer-lasting pain relief than salt water because it forms a protective coating over sores. Salt water rinses help clean the area and reduce bacteria, but they don’t numb pain or shield the tissue. Many patients use both: salt water for cleaning, Gelclair for pain.
Why is ice chips recommended only for some chemo drugs?
Cryotherapy works best with short-infusion drugs like melphalan and 5-fluorouracil because the cold only protects tissue during the time the drug is in your bloodstream. For drugs given over hours or days - like continuous infusions - ice chips won’t help. Your care team will tell you if your regimen qualifies.
Can I use regular mouthwash if I have mouth sores?
No. Most commercial mouthwashes contain alcohol, which burns open sores and makes pain worse. Avoid anything with alcohol, peroxide, or strong flavors. Stick to baking soda rinses, water, or prescribed solutions like benzydamine or dexamethasone.
How long do medication-induced mouth sores last?
They usually start 5-10 days after treatment begins and peak around day 10-14. Without prevention, they can last 2-4 weeks. With proper care, healing often happens in 7-14 days. The key is not waiting until they’re bad - start prevention before treatment begins.
Are there any natural remedies that work?
Honey has shown some benefit in small studies - especially medical-grade Manuka honey - for soothing sores. But don’t rely on it alone. Avoid turmeric, aloe vera, or essential oils unless your oncologist approves them. Many natural products aren’t tested for safety during cancer treatment and could interfere with your therapy.

Julie Pulvino
November 24, 2025 AT 11:00I started using ice chips during my chemo sessions last year and honestly? Life-changing. Didn’t think it would work, but I stuck with it-5 minutes before, 30 after, no exceptions. The pain wasn’t gone, but it was manageable. I even got my mom to do it with me. She cried when I told her it helped. We both felt like we were doing something real.
Patrick Marsh
November 24, 2025 AT 11:20Don't use benzocaine. FDA warning. Period.
Danny Nicholls
November 26, 2025 AT 05:30Benzydamine saved me during radiation 😭 I used it 3x a day like clockwork. Stung like hell at first, but after day 3? I was actually looking forward to swishing. My dentist said I was the first patient in 5 years who didn’t need a feeding tube. Also, SLS-free toothpaste? Non-negotiable. I switched to Tom’s of Maine and my mouth stopped feeling like sandpaper. 🙌
Robin Johnson
November 27, 2025 AT 06:33People skip dental checkups because they think it’s ‘not urgent.’ But if you’re getting chemo or radiation, your mouth is ground zero. A loose filling or infected gum can turn into a hospital trip. I had mine done 3 weeks before starting. No sores. No infections. Just peace of mind. Don’t wait until it’s too late. Your oncologist won’t remind you. You have to push for it.
Latonya Elarms-Radford
November 27, 2025 AT 10:30It’s ironic, isn’t it? We’re told that modern medicine can cure cancer-yet the very tools meant to save us carve open our mouths like a butcher’s knife. We’re not just patients-we’re collateral damage in a war against cells that don’t know the difference between good and evil. And yet, we’re expected to smile through it, to ‘stay positive,’ as if our suffering is a performance for the nurses. Gelclair? It’s a bandage on a gunshot wound. Cryotherapy? A temporary reprieve. We’re being asked to manage symptoms of a system that refuses to fix the root cause: that chemotherapy is still a blunt instrument in a world that needs precision.
Mark Williams
November 28, 2025 AT 01:46GC4419’s phase 3 results are promising-superoxide dismutase mimetic activity reduces ROS-mediated epithelial apoptosis, which directly correlates with mucositis severity. The 38% reduction in duration aligns with prior murine models showing Nrf2 pathway modulation. Still, cost and accessibility remain barriers. LLLT at 650nm/40mW shows photobiomodulation effects on fibroblast proliferation-potential for outpatient protocols. But until personalized risk stratification is integrated into EHRs, we’ll keep seeing one-size-fits-all protocols that fail high-risk subgroups.
Justin Daniel
November 29, 2025 AT 13:40Glutamine? I tried it. Swished for 2 minutes, swallowed like they said. Didn’t feel much. But my buddy swears by it-he’s been on it for 8 months now. Maybe it’s placebo, maybe not. Either way, it’s cheap and safe. Why not? I’m not gonna argue with a $15 jar of powder that might help. Also, Biotene? Lifesaver for dry mouth. I keep a bottle in my car, my purse, my nightstand. It’s like oxygen for your mouth.
Melvina Zelee
December 1, 2025 AT 01:02ice chips are kinda weird but i tried them and honestly? they work. my mouth felt like it was on fire during chemo and then i just started sucking on ice like a popsicle and it was like… a tiny win? i didn’t cry as much. also i switched to a baby toothbrush and it felt like a hug for my gums. no more bleeding. i think i love my toothbrush now. 🥺
Holly Schumacher
December 2, 2025 AT 23:00Let me be clear: if you’re not using palifermin and you’re undergoing a stem cell transplant, you’re doing it wrong. The data is irrefutable. A 63% to 20% reduction in severe mucositis? That’s not a ‘maybe’-it’s a standard of care. The fact that 92% of uninsured patients can’t afford it speaks volumes about the brokenness of this system. You don’t get to say ‘prevention is key’ while charging $10,500 for a drug that literally prevents suffering. This isn’t medicine. It’s extortion dressed in white coats.
Michael Fitzpatrick
December 4, 2025 AT 08:12I’ve been through this twice now. First time, I ignored everything. Got hospitalized. Second time, I did the ice chips, the benzydamine, the SLS-free toothpaste, the baking soda rinses. Didn’t get one ulcer that needed pain meds. It’s not magic. It’s just… doing the work. I wish I’d known this stuff the first time. I wasted so much time thinking it was just ‘part of the process.’ It’s not. It’s preventable. And you deserve to not hurt.
Shawn Daughhetee
December 4, 2025 AT 13:09just use gelclair and forget the rest. it works. i dont care what the studies say. my mouth stopped screaming. that’s all i need.
Miruna Alexandru
December 5, 2025 AT 19:00While the article cites MASCC/ISOO guidelines, it fails to acknowledge the conflict-of-interest disclosures of several authors who have received funding from pharmaceutical companies that manufacture benzydamine and Gelclair. The promotion of these products as ‘gold standard’ lacks critical scrutiny. Additionally, the dismissal of chlorhexidine as ‘overused’ contradicts WHO recommendations for immunocompromised populations. This reads less like evidence-based medicine and more like a marketing pamphlet disguised as patient advocacy.
ann smith
December 7, 2025 AT 13:17Thank you for writing this. I’ve been waiting for someone to say it plainly: you don’t have to suffer. I showed this to my oncologist and she actually changed my care plan. We added cryotherapy and benzydamine. I still have bad days. But now I feel like I have tools. Not just a pill to numb the pain. Real things I can do. I’m not just a patient anymore. I’m someone who fights back. 💪