Monitoring While on Statins: Lab Tests and Safety Considerations
 Feb, 20 2026
Feb, 20 2026
Statins Safety Checker
Enter Your Test Results
Your Results
Enter your test results to see guidance
Important Note
THIS TOOL IS FOR INFORMATIONAL PURPOSES ONLY AND DOES NOT SUBSTITUTE FOR MEDICAL ADVICE. ALWAYS CONSULT YOUR PHYSICIAN FOR PERSONALIZED MEDICAL DETERMINATIONS.
When you start taking a statin, it’s not just about popping a pill and forgetting about it. You need to know what to watch for - and more importantly, what not to worry about. Many people are told to get blood tests every few months, but that’s often unnecessary. The science has changed. So have the guidelines. And if you’re still getting monthly liver tests because your doctor “just wants to be safe,” you’re not alone - but you might be getting tested more than you need to.
What Statins Actually Do
Statins are among the most studied drugs in medical history. They work by blocking an enzyme in your liver called HMG-CoA reductase, which your body uses to make cholesterol. The goal? Lower LDL (bad) cholesterol by 30% to 50%, depending on the statin and dose. That drop cuts your risk of heart attack and stroke. For millions of people, statins are life-saving.
But like all medicines, they come with possible side effects. The big ones people worry about are liver damage and muscle pain. That’s why monitoring has been a standard part of care - for decades. But here’s the twist: most of that monitoring was never backed by solid evidence.
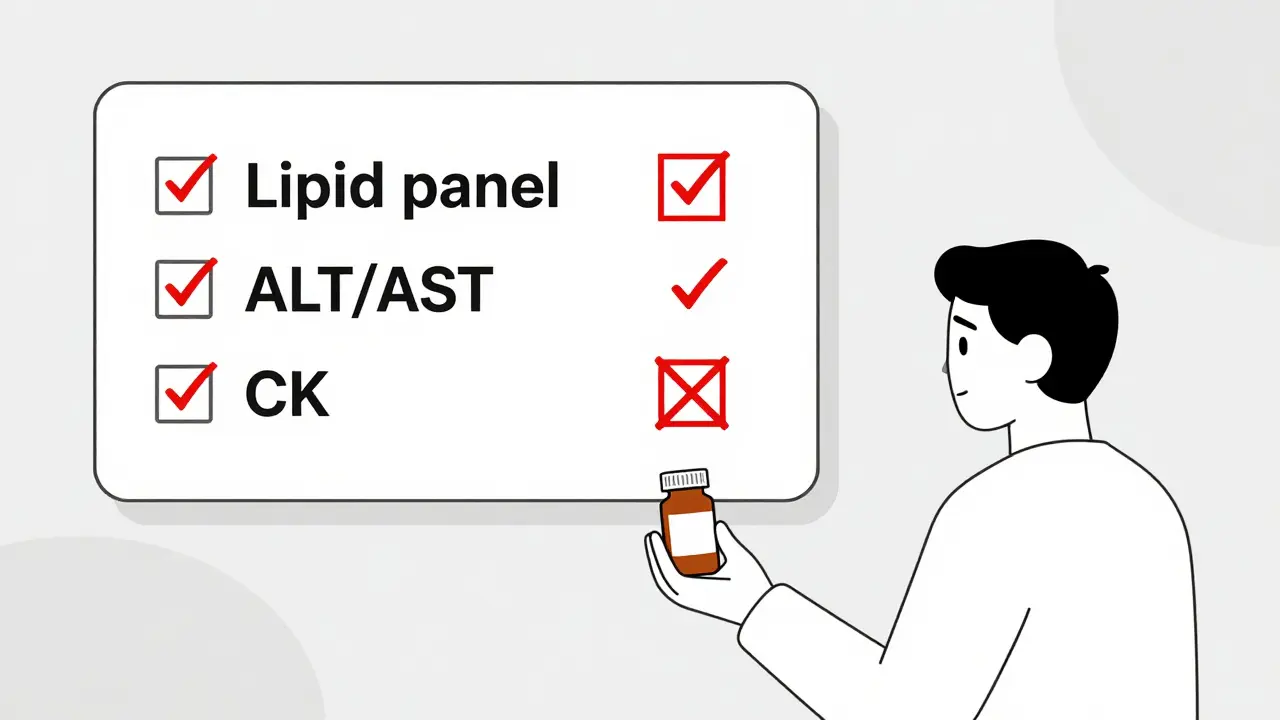
What Lab Tests Actually Matter
Let’s cut through the noise. You don’t need a full panel every time you visit your doctor. Here’s what actually matters:
- Lipid panel - This is the only test you need regularly. It checks total cholesterol, LDL, HDL, and triglycerides. Do this 4 to 12 weeks after starting or changing your statin dose. Then repeat every 3 to 12 months. The goal? See if LDL dropped by at least 30%. If not, your dose might need adjusting.
- Liver enzymes (ALT/AST) - Get these once before you start. Then again at 3 months. Then once at 12 months. After that? Only if you have symptoms like dark urine, yellow eyes, or unexplained fatigue. Routine testing beyond that adds zero safety benefit. The FDA removed the requirement for regular liver tests in 2012 after reviewing 83,000 patients across 33 studies. Not one serious liver injury was linked to statin use in the placebo group.
- Creatine kinase (CK) - This measures muscle damage. Only test this if you have persistent muscle pain, weakness, or cramps that don’t go away. Don’t test it after a workout - intense exercise alone can spike CK levels. If CK is more than 10 times the normal range, stop the statin. Below that? Keep going unless symptoms worsen.
- Kidney function and HbA1c - These are checked at baseline, especially if you have diabetes risk factors (obesity, high blood pressure, prediabetes). But you don’t need to repeat HbA1c every few months just because you’re on a statin. The American Diabetes Association says monitor it based on your diabetes status, not your statin use.
Why So Many Doctors Still Order Too Many Tests
It’s not that doctors are wrong. It’s that habits die hard.
In 2012, the FDA updated its guidelines: no more routine liver tests. NICE (UK), the ACC/AHA (US), and the National Lipid Association all followed. But here’s what happened next: electronic health records (EHRs) kept auto-populating quarterly liver tests. Patients got letters. Doctors got reminders. And many just kept ordering them out of habit.
A 2020 survey found 78% of U.S. healthcare systems still had default EHR orders for quarterly liver tests. Even worse - 38% of providers still order them every 3 months. That’s not just outdated. It’s costly. In the U.S. alone, unnecessary liver tests cost over $1.2 billion a year.
And here’s the real danger: people stop their statins because of a slightly high liver test. One study in JAMA Internal Medicine found that patients who stopped statins over minor enzyme elevations had a 10% to 20% higher risk of heart attack or stroke. That’s not safety. That’s harm.

When to Be Concerned - And When Not To
Not every abnormal result means you should quit statins.
- ALT or AST is 1.5 to 3 times the normal range? Ignore it. These small rises are common, temporary, and harmless. They don’t predict liver damage. Recheck in a month. If it’s still up, check again. If it’s still up after two months? Talk to your doctor. But don’t stop the statin.
- ALT or AST is more than 3 times normal? This is the threshold where you pause the statin. But even then, most cases resolve on their own. Restarting the same or a different statin often works fine.
- Muscle pain? Not every ache means myopathy. If your pain is mild and goes away with rest, keep taking it. If it’s constant, deep, or makes it hard to climb stairs or lift your arms - then get CK tested. And skip the gym for a few days before the test.
- Diabetes risk? Statins slightly raise blood sugar in some people. But the heart benefits far outweigh this small risk. Don’t skip statins because you’re worried about diabetes. Just check HbA1c once a year if you’re at risk.
Who Needs Extra Monitoring?
Not everyone follows the same rules. Some people need more attention:
- You’re on both a statin and a fibrate (like fenofibrate). This combo increases muscle risk.
- You have pre-existing liver disease (like hepatitis or fatty liver).
- You have kidney disease (eGFR below 30).
- You’re over 75 and taking a high-intensity statin (like rosuvastatin 20mg or atorvastatin 40mg).
- You’re taking other drugs that interact with statins - like certain antibiotics, antifungals, or grapefruit juice in large amounts.
If any of these apply to you, your doctor may want to check liver or muscle markers more often. But even then, it’s not every 3 months. It’s based on your situation.
The Future: Personalized Monitoring
Science is moving toward smarter monitoring. In 2023, the FDA approved new guidelines for a genetic test called SLCO1B1. If you have a certain variant, you’re more likely to get muscle pain on simvastatin. Testing for this can help pick a safer statin upfront.
Another shift? Measuring ApoB instead of LDL. It’s a better predictor of risk, especially if your triglycerides are high. Some lipid specialists now use ApoB as their main target.
By 2027, AI tools may automatically flag patients who need closer monitoring based on their EHR data - age, other meds, lab trends, symptoms. That means fewer blanket tests for healthy people, and more focus on those who truly need it.
What You Should Do Right Now
Here’s your simple action plan:
- Ask your doctor: “What tests do I actually need, and when?”
- Get your baseline lipid panel and liver enzymes before starting the statin.
- Get another lipid panel 8 to 12 weeks after starting.
- Get liver enzymes again at 3 months and 12 months.
- After that? Only test if you feel unwell - not because someone told you to.
- Keep a log of muscle pain, fatigue, or dark urine. Bring it up if it lasts more than a week.
If your doctor insists on quarterly liver tests, show them the 2018 ACC/AHA guidelines or the 2012 FDA update. You’re not being difficult - you’re being informed.
Common Misconceptions Debunked
- Myth: Statins cause liver damage. Truth: Severe liver injury from statins is rarer than being struck by lightning. Less than 1 in a million people per year.
- Myth: All muscle pain means statin myopathy. Truth: Most muscle pain in statin users is unrelated. It’s often from aging, inactivity, or other meds.
- Myth: I need HbA1c every 3 months. Truth: Only if you have diabetes or prediabetes. Statins alone don’t require it.
- Myth: If my ALT is high, I have to stop the statin. Truth: Only if it’s over 3 times normal and stays there. Even then, restarting often works.
Do I need to get blood tests every 3 months on statins?
No. Routine testing every 3 months is outdated. You only need liver tests at baseline, 3 months, and 12 months. Lipid panels should be checked 4 to 12 weeks after starting, then every 3 to 12 months. Beyond that, only test if you have symptoms.
Can statins cause liver damage?
Severe liver damage from statins is extremely rare - less than one case per million patient-years. Minor, temporary rises in liver enzymes are common and harmless. They don’t predict injury. The FDA removed routine liver monitoring in 2012 because evidence showed no benefit.
I have muscle pain. Should I stop my statin?
Not necessarily. Mild, occasional muscle aches are common and usually not related to statins. If the pain is persistent, deep, and affects daily movement (like climbing stairs), get a creatine kinase (CK) test. Only stop the statin if CK is more than 10 times the normal level. Otherwise, talk to your doctor - switching to a different statin often helps.
Why do some doctors still order monthly liver tests?
Many doctors learned outdated protocols and haven’t updated their practice. Electronic health records often auto-schedule quarterly tests. Some are afraid of missing a rare side effect. But research shows this leads to more harm than good - including unnecessary statin discontinuation, which raises heart attack risk.
Is there a genetic test for statin side effects?
Yes. The SLCO1B1 gene test identifies people at higher risk for muscle side effects from simvastatin. About 12% of Caucasians carry this variant. Testing isn’t routine yet, but it’s available and may help choose a safer statin upfront. Ask your doctor if it’s right for you.

Tommy Chapman
February 20, 2026 AT 14:32Ugh, I can't believe doctors are still ordering liver tests every 3 months like it's 2005. I've been on statins for 8 years and they used to bug me for bloodwork like I was a lab rat. Then I read the FDA guidelines myself and shut that down. My PCP was mad, but I showed her the 83,000-patient study. She stopped. Now I just get lipid panels once a year. Why are we still doing this? It's not medicine-it's fear-based billing. And don't get me started on EHRs auto-populating tests like they're Christmas wishlists.