Managing Warfarin and Antibiotics: Common Interaction Issues
 Nov, 1 2025
Nov, 1 2025
Warfarin-Antibiotic Interaction Checker
Check Antibiotic Safety
Enter the antibiotic name to see its interaction risk level with warfarin and recommended actions.
Risk Level:
INR Effect:
Monitoring:
Dose Adjustment:
Key Actions:
When you're on warfarin, even a simple course of antibiotics can throw your blood thinning off balance. It’s not rare. About 20-30% of people taking warfarin end up on antibiotics each year - for a sinus infection, a urinary tract infection, or even dental work. But here’s the catch: mixing these two can spike your INR dangerously high, raising your risk of internal bleeding. Or, in some cases, it can drop your INR too low, putting you at risk for a clot. The good news? You don’t need to avoid antibiotics. You just need to know what to watch for - and when to act.
Why Warfarin and Antibiotics Don’t Play Nice
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. But your gut bacteria also make vitamin K - about 10-15% of what your body uses. When you take antibiotics, especially broad-spectrum ones, you kill off those helpful bacteria. Less vitamin K means warfarin works harder than usual. Your INR climbs. That’s the most common reason for trouble. But that’s not the only way antibiotics interfere. Some directly block the liver enzyme CYP2C9, which breaks down warfarin. When that enzyme slows down, warfarin builds up in your blood. Other antibiotics compete for protein binding sites, briefly increasing the amount of free, active warfarin in your bloodstream. And then there’s rifampin - the exception. It does the opposite: it speeds up warfarin breakdown, making it less effective.Which Antibiotics Are Riskiest?
Not all antibiotics are created equal when it comes to warfarin interactions. Some are red flags. Others? Barely a blip.- High-risk antibiotics: These can raise your INR by more than 1.5 units in many patients. Trimethoprim-sulfamethoxazole (Bactrim, Septra) is the biggest offender. Studies show it triples your risk of bleeding. Fluconazole (an antifungal) is nearly as dangerous. If you’re on one of these, expect your doctor to cut your warfarin dose by 25-50% - sometimes even skip a dose.
- Moderate-risk antibiotics: These include ciprofloxacin, levofloxacin, erythromycin, amoxicillin, and cephalexin. They typically raise INR by 0.5 to 1.5 units. A 10-25% warfarin reduction is often needed, but not always. Monitoring is key.
- Low-risk antibiotics: Clindamycin and azithromycin barely touch warfarin. In fact, dentists often choose clindamycin for patients on warfarin because it’s the safest option. Azithromycin is also low-risk, unlike its cousin erythromycin.
- The outlier: Rifampin. This one doesn’t raise INR - it drops it. Rifampin speeds up how fast your liver clears warfarin. Your INR can fall below target in days. You’ll likely need a 50-100% increase in your warfarin dose. And it takes 6-8 weeks for things to stabilize.
When to Check Your INR
The rule of thumb? Check your INR within 3 to 5 days after starting any antibiotic. That’s when the biggest changes happen. Don’t wait until your next scheduled test. Don’t assume you’re fine because you feel okay. Bleeding can happen silently - a bruise that won’t fade, dark stools, a headache that won’t quit. For high-risk antibiotics like Bactrim, check at day 3. For moderate ones like ciprofloxacin or amoxicillin, day 5 is fine. For low-risk ones like clindamycin, stick to your normal schedule unless you notice unusual bruising or bleeding. And don’t forget: the effect can last days after you stop the antibiotic. Keep checking INR for another 3-7 days after finishing the course. Your body needs time to rebuild gut bacteria and reset vitamin K levels.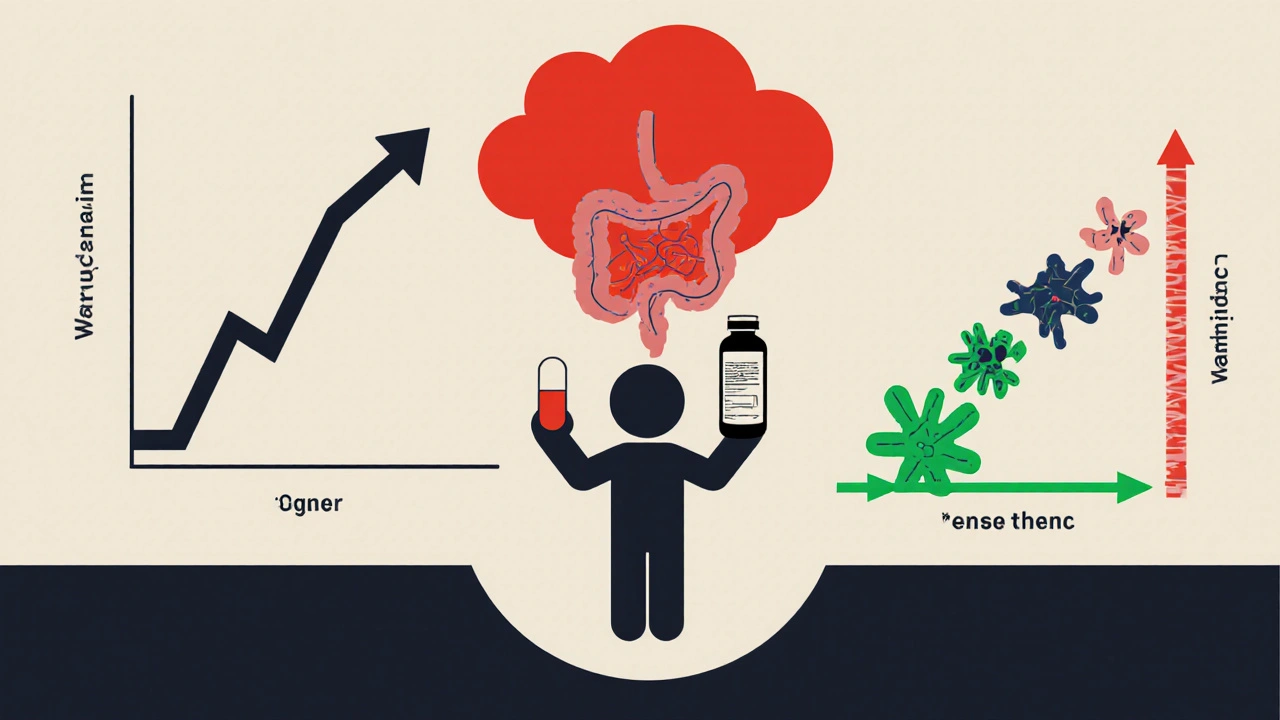
What Your Doctor Will Do
Your doctor won’t stop your warfarin. They won’t stop your antibiotic. They’ll adjust the dose - and they’ll watch you closely. If your INR spikes above 4.0, especially if you’re over 65 or have a history of bleeding, your doctor might:- Hold your next warfarin dose
- Give you a small amount of vitamin K orally (not an injection)
- Check INR again in 24 hours
Real-Life Scenarios
Imagine you’re 72, on warfarin for atrial fibrillation. You get a UTI. Your doctor prescribes Bactrim. Within 48 hours, you notice your gums bleed when you brush. You call your anticoagulation clinic. They check your INR - it’s 6.2. They hold your next warfarin dose, give you 1 mg of oral vitamin K, and schedule a repeat INR in 24 hours. You’re monitored closely. No hospital stay. No clot. Just smart management. Or picture a 58-year-old with a mechanical heart valve. They need antibiotics before a dental cleaning. Their dentist suggests clindamycin. The INR stays stable. No dose change. No panic. Just the right choice. Now think of someone on rifampin for tuberculosis. Their INR drops from 2.5 to 1.6 after a week. Their warfarin dose is increased from 5 mg to 8 mg. They’re checked weekly. It takes six weeks, but they stabilize. No stroke. No bleed.
What You Can Do
You’re not powerless here. Here’s what actually works:- Always tell every doctor and pharmacist you’re on warfarin. Even for a cold or a rash. Don’t assume they know.
- Keep a log. Write down every antibiotic you take - name, dose, start and end date. Note any unusual bruising, bleeding, or symptoms.
- Don’t self-medicate. Over-the-counter painkillers like ibuprofen or naproxen can also raise bleeding risk. Stick to acetaminophen (Tylenol) unless your doctor says otherwise.
- Ask about alternatives. If you need antibiotics, ask: "Is there a lower-risk option?" For dental work, clindamycin is often the go-to.
- Know your target INR. Most people are between 2.0 and 3.0. Know your range. If you’re on it for a mechanical valve, it might be higher.
Myth vs. Reality
There’s a lot of fear around this. Let’s clear up the noise.- Myth: You can’t take antibiotics on warfarin. Reality: You can - as long as you’re monitored.
- Myth: All antibiotics cause bleeding. Reality: Only some do. Clindamycin and azithromycin are safe for most.
- Myth: If you feel fine, your INR is fine. Reality: Bleeding can happen without symptoms. INR is the only reliable measure.
- Myth: Once the antibiotic stops, everything goes back to normal. Reality: It can take days to weeks for gut bacteria to recover. Keep monitoring.
Bottom Line
Warfarin and antibiotics can be managed safely. It’s not about avoiding one or the other. It’s about awareness, timing, and communication. The risk of bleeding from this interaction is real - but it’s predictable. And it’s preventable. If you’re on warfarin and need antibiotics, don’t panic. Do this:- Call your anticoagulation clinic or doctor before starting the antibiotic.
- Get your INR checked 3-5 days after starting.
- Follow their instructions on dose changes - don’t adjust it yourself.
- Watch for signs of bleeding: unusual bruising, nosebleeds, blood in urine or stool, severe headaches.
- Keep taking your warfarin unless told otherwise. Stopping it can cause clots - which are just as dangerous.
Can I take amoxicillin while on warfarin?
Yes, you can take amoxicillin while on warfarin, but your INR may rise slightly. Amoxicillin is considered a moderate-risk antibiotic. Your doctor will likely recommend checking your INR 5 to 7 days after you start the antibiotic. A small dose reduction (10-25%) may be needed, but many patients don’t require any change. Always monitor - don’t assume it’s safe just because it’s a common antibiotic.
Is clindamycin safe with warfarin?
Yes, clindamycin is one of the safest antibiotics to use with warfarin. It has minimal effect on CYP2C9 enzymes and doesn’t significantly disrupt vitamin K-producing gut bacteria. Studies and clinical guidelines, including those from dental associations, recommend clindamycin as a first-choice antibiotic for patients on warfarin, especially before dental procedures. No routine INR adjustment is needed unless you notice unusual bleeding.
How long does it take for warfarin to return to normal after antibiotics?
It usually takes 3 to 10 days after stopping the antibiotic for your INR to stabilize. The exact time depends on the antibiotic and your gut microbiome recovery. For high-risk drugs like Bactrim, INR can stay elevated for up to two weeks. Monitor your INR every few days after finishing the antibiotic until it returns to your target range. Don’t rush to increase your warfarin dose - let your body rebalance naturally.
What should I do if my INR is too high?
If your INR is above 4.0, contact your doctor immediately. Do not stop warfarin on your own. For INR between 4.0 and 10.0, your doctor may hold your next dose and give you a small amount of oral vitamin K. If your INR is above 10, or if you’re bleeding, seek emergency care. Never take vitamin K without medical advice - too much can make warfarin ineffective and increase clot risk.
Can I use ibuprofen for pain while on warfarin and antibiotics?
No. Ibuprofen and other NSAIDs like naproxen increase bleeding risk when combined with warfarin - even without antibiotics. Stick to acetaminophen (Tylenol) for pain or fever. NSAIDs can irritate your stomach lining and interfere with platelet function, making bleeding more likely. This risk is amplified when you’re on antibiotics that also affect your INR. Always check with your doctor before taking any new medication.

Marshall Washick
November 3, 2025 AT 01:18I was on warfarin for AFib and got prescribed amoxicillin for a sinus infection. Didn't think twice until my gums started bleeding like a faucet. Called my anticoag clinic on day 4 - INR was 5.8. They held my dose and gave me 1mg oral vit K. No hospital, no panic. Just a quick call and a little patience. This post? Lifesaver. I wish I'd read it before I started the antibiotic.
Abha Nakra
November 3, 2025 AT 09:36As a pharmacist in India, I see this every week. Patients come in panicked because their doctor prescribed ciprofloxacin and they’re scared to take it. I always explain: it’s not about avoiding antibiotics - it’s about timing. Check INR at day 5. Most don’t need a dose change. But if you skip the check, you’re gambling with your life. Clindamycin? My go-to for dentists. Safe, simple, no drama. Warfarin patients deserve better than fear - they deserve clarity.
Neal Burton
November 4, 2025 AT 00:36Look, this is why medicine is a joke. You’re telling people to monitor INR after antibiotics like it’s some kind of magic ritual. The truth? The entire anticoagulation system is a house of cards built on outdated protocols and profit-driven guidelines. Why aren’t we using DOACs instead of this archaic warfarin nonsense? Because the pharmaceutical industry makes billions off INR tests and vitamin K vials. This isn’t safety - it’s a revenue stream disguised as care.
Tamara Kayali Browne
November 5, 2025 AT 00:35While the article contains clinically accurate information, it lacks critical nuance regarding pharmacokinetic variability across ethnic populations. For instance, Indian and East Asian patients often exhibit reduced CYP2C9 activity, leading to exaggerated INR elevation even with moderate-risk antibiotics. The generalization of "moderate-risk" without stratification by genotype or ancestry is misleading and potentially hazardous. Furthermore, the recommendation to use oral vitamin K at INR >4.0 contradicts the 2021 ACCP guidelines, which advise against routine vitamin K unless INR >10 or active bleeding. This post, while well-intentioned, risks reinforcing therapeutic misinformation.
Nishigandha Kanurkar
November 6, 2025 AT 01:46WAIT - THEY’RE HIDING THE TRUTH!!! BACTRIM ISN’T THE PROBLEM - IT’S THE VITAMIN K SUPPLEMENTS THEY’RE PUSHING ON YOU!! THEY’RE USING ANTIBIOTICS TO MAKE YOU RELY ON WARFARIN SO THEY CAN KEEP SELLING YOU INR TESTS!! AND RIFAMPIN? THAT’S A COVER-UP - THEY WANT YOU TO THINK IT LOWERS INR SO YOU’LL KEEP TAKING WARFARIN LONGER!! THE GUT BACTERIA THEORY? A LIE! THEY’RE INJECTING FLUORIDE INTO THE WATER TO DESTROY YOUR LIVER AND MAKE YOU DEPENDENT ON DRUGS!! CHECK YOUR WATER FILTER!! THEY’RE LYING TO YOU!!
Lori Johnson
November 7, 2025 AT 04:16Hey, I just wanted to say thank you for writing this - I’m a nurse and I’ve seen so many patients get scared off antibiotics because of this. One lady thought she couldn’t take amoxicillin for a UTI and ended up with pyelonephritis. I printed out this exact guide and gave it to her. She cried. Said she felt like someone finally understood. You’re right - it’s not fear, it’s control. And you gave people the tools. I’m sharing this with my whole unit.
Tatiana Mathis
November 7, 2025 AT 20:14This is one of the clearest, most practical summaries I’ve seen on this topic - and I’ve read dozens of guidelines. The breakdown of antibiotic risk levels is spot-on, especially highlighting clindamycin as a low-risk option. I’ve been managing warfarin for over a decade, and I still learned something: the 3-7 day post-antibiotic monitoring window. I always assumed stabilization happened immediately after stopping the drug. Also, the myth-busting section? Perfect. So many patients think "if I feel fine, I’m fine" - and that’s how strokes happen. The real hero here is the patient who calls their clinic proactively. That’s the behavior we need to normalize. Thank you for writing this. I’m saving it for my next patient education packet.
Michelle Lyons
November 8, 2025 AT 02:50Did you know that the FDA doesn’t require antibiotic manufacturers to test interactions with warfarin? That’s because they’re paid off by Big Pharma. Every time you take an antibiotic, you’re being used as a guinea pig. The INR test? It’s not for your safety - it’s to make sure you keep coming back for more blood draws. They want you dependent. They want you scared. Don’t trust your doctor. Don’t trust your pharmacist. Check your own INR with a home monitor - and if you see any spike, stop everything and go off-grid. They’re watching you.
Cornelle Camberos
November 8, 2025 AT 23:57It is imperative to underscore that the pharmacodynamic interactions between warfarin and antibiotics constitute a Class I clinical concern, as defined by the American College of Clinical Pharmacy. The assertion that clindamycin is "safe" is, while generally accurate, an oversimplification. In patients with hepatic impairment or concurrent use of CYP3A4 inhibitors, even low-risk agents may precipitate clinically significant INR elevation. Furthermore, the temporal window for INR monitoring must be individualized based on baseline renal function, age, and concomitant medications. The recommendation to check INR at day 3 or 5 lacks granularity and may result in suboptimal clinical outcomes. This discourse, while well-intentioned, must be contextualized within the framework of precision medicine - not generalized protocol.