Lipitor: The Complete Guide to Cholesterol Control and Heart Health
 May, 25 2025
May, 25 2025
If there’s one pill that made drug history in the last 25 years, it’s Lipitor. By 2012, it had raked in over $125 billion, making it the highest grossing prescription drug worldwide. But it’s not about the money—Lipitor, or atorvastatin, became a household name because it changed the way doctors fight high cholesterol. Imagine a medication so widely trusted that it’s prescribed to millions, every single year, with the goal of saving people from heart attacks and strokes. Yet, talk to a few friends and you’ll hear everything from rave reviews to worried stories about muscle pain. So, what's hype and what's fact when it comes to Lipitor?
What is Lipitor, and How Does it Really Work?
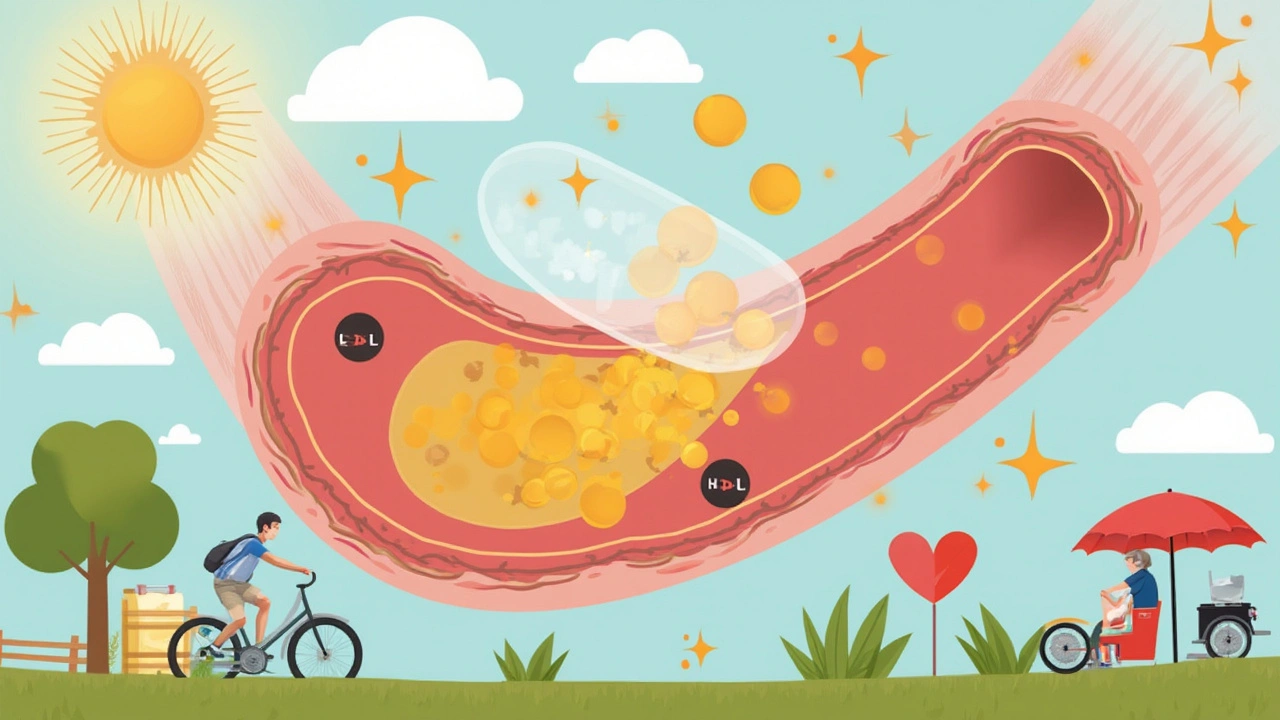
For starters, Lipitor is part of a group of medications called statins. These drugs help your body lower its LDL, or "bad cholesterol." That matters, because LDL cholesterol loves to stick to artery walls, turn into plaque, and block blood flow. When arteries get blocked, your risk for heart attacks and strokes goes up fast.
Lipitor’s main job is to block an enzyme in your liver—HMG-CoA reductase—that your body uses to make cholesterol. It’s a bit like shutting off a machine at the factory so less product gets out the door. The result? LDL cholesterol in your blood starts to drop, sometimes by as much as 60%.
But it’s not just one number Lipitor changes. It often helps bump up your HDL, the "good" cholesterol, and can cut triglycerides too. This three-way combo gives your arteries a better shot at staying clear. No other class of cholesterol drugs has racked up as much evidence in preventing heart problems. There are studies with thousands—and sometimes, hundreds of thousands—of people proving that statins, especially Lipitor, lower risk for heart attacks and strokes.
Want some real numbers? Here’s a look at how Lipitor’s performance compares in clinical trials—check out the table below:
| Outcome | Reduction with Lipitor | Typical Study (Duration) |
|---|---|---|
| LDL Cholesterol | 38-60% drop | ASCOT-LLA (3 years) |
| Heart Attack Risk | 36% lower | TNT (5 years) |
| Stroke Risk | 27% lower | SPARCL (5 years) |
| Total Deaths | 12% lower | PROVE-IT (2 years) |
Doctors trust Lipitor because it has proven effects, and not just in folks with sky-high cholesterol. If you’ve already had a heart attack or if you have diabetes, Lipitor often ends up in your medicine cabinet, sometimes even before your cholesterol numbers look bad. Some doctors call this "secondary prevention"—protecting people who already dodged a bullet from having another close call.
So, if you're wondering what sets Lipitor apart and why it became such a medical staple, think simplicity. It's taken once a day, works in nearly everyone, and can make a serious difference in how long, and how well, you live. Some foods and drugs can mess with how Lipitor works, though, so you can’t just pop it on your own schedule without a chat with your doctor. Grapefruit is a classic example—just one glass of juice can change how much Lipitor gets absorbed, and sometimes that’s not a good thing.
Here’s something most folks don’t realize: you won’t feel any different when your cholesterol drops. There are no fast "before and after" tricks like you’d see in gym ads. Most people get put on Lipitor because their numbers are off, not because they feel lousy. That can make it easy to forget your pill, especially since cholesterol is a silent threat. Keeping a schedule, setting reminders, or tying your pill time to another habit (like brushing your teeth) makes a huge difference in staying on track.
Okay, so what if your cholesterol isn’t crazy high? Your doctor might still talk about starting Lipitor if you’ve got high blood pressure, a family history of heart problems, diabetes, or if you smoke. The latest guidelines push doctors to look at your whole risk picture, not just your cholesterol number. Still, the main goal is pretty simple: keep those fatty blockages away while you go about your day.

Who Benefits Most from Lipitor?
Reading the stats on Lipitor, it sounds like everyone should be taking it. But that’s not the case. The real gains happen for certain groups, and doctors spend a lot of time figuring out who gets the most out of this little white pill.
If you’ve already had a heart attack or stroke, Lipitor is almost a no-brainer unless there’s a strong reason against it. It’s the front-line choice for people who’ve shown a sign of heart trouble. But the benefits go farther. If you have type 2 diabetes—even without a personal history of heart disease—your risk still jumps, and that makes you a strong candidate for starting Lipitor. Same goes for people with super high LDL cholesterol, usually over 190 mg/dL (that’s very high), even if their blood pressure and blood sugar look great.
Say you’re just a regular person, late 40s, maybe a little overweight but not diabetic, and no scars from a heart attack or stroke. The decision now depends on your constellation of risk: How’s your blood pressure? Do you smoke? Does mom or dad have a heart problem history? There’s actually a risk calculator that doctors use, factoring in your age, sex, race, cholesterol levels, and even whether you’re on blood pressure treatment. If your chances of a heart attack top 7.5% in the next decade, odds go way up that your doctor will mention Lipitor.
This calculator might sound like just more doctor stuff, but it really is a tool that helps take the guesswork out. A funny thing here—plenty of guys in their 30s and 40s think heart attacks are decades away, but genetics and smoking can load the dice early. It’s not rare for men under 50 to land on statins, sometimes as a wake-up call if their LDL is stubbornly high.
A lot of people wonder: is there such a thing as starting too early? You shouldn’t be jumping on Lipitor if you’re healthy, young, and don’t have risk. The drug is safe, but nobody wants to take medicine unless there’s real benefit. Part of the art here is knowing if lifestyle fixes, like food swaps or more steps each day, can get you to a safe cholesterol level before you need meds. But the honest truth—diet and exercise don’t move the needle as fast or as far as Lipitor does for most people with very high cholesterol or a big risk score. Sometimes, it’s a “both/and,” not an “either/or.”
Kids and teens almost never get Lipitor, but there are rare genetic conditions that cause cholesterol to spike early in life—familial hypercholesterolemia, for example. In those cases, specialists may bring statins into the picture sooner, but that’s not most families’ situation.
Guess what group sometimes doesn’t benefit as much, or faces extra risks? Older adults, especially those over 75, sometimes need a different conversation with their doctor. That’s because the benefit of cholesterol lowering in people with shorter life expectancy can be less clear, and some older people deal with a higher risk of side effects. Still, if an older person is healthy and has a good shot at living another 10 years, statins stay a smart option.
Pregnant women, though, should never be on Lipitor. It can harm a developing baby, so anyone who is pregnant or planning should steer clear. If you’re a woman of childbearing age, birth control and a good talk with your doctor are musts if you’re prescribed Lipitor.
What about people with really bad liver disease? Since Lipitor works in the liver, those with serious liver trouble often have to avoid it or get special monitoring. Liver tests are run before starting and sometimes during, just to catch any rare issues before they turn big.
In short, Lipitor is a game-changer for people with high risk, those with a history of heart or vessel problems, folks with diabetes, and anyone who’s struggling with sky-high cholesterol, despite their best efforts at lifestyle changes. Knowing your numbers, family history, and real-life risks goes a long way in making the call.
Side Effects, Safety Myths, and Practical Tips for Taking Lipitor
Now for the tricky part—every medicine comes with stories, and Lipitor is no exception. The most common side effect you hear about is muscle pain. That’s not a myth. Up to 10% of people notice aching, soreness, or fatigue, especially in their legs. But, only about 1 in 100 actually has to stop the drug because of it. The vast majority push past the aches or find that the pains fade after a few weeks. There are rare, serious muscle problems—like rhabdomyolysis—but these are much less common with Lipitor than with older statins or super-high doses. If you do develop unexplained muscle pain, especially with dark urine or a fever, call your doctor right away. Most of the time, changing the dose or switching statins can help.
Some folks are wary of the liver effects. Honestly, true liver problems linked to Lipitor are rare (about 1 in 10,000 people). Your doctor checks your liver blood tests before and sometimes after you start. As a tip, watch out for yellowing of your skin or eyes and call your doc if that shows up, but don’t expect it—it’s really uncommon.
Ever heard statins cause memory loss? Early reports were alarming, but bigger studies since found no link between Lipitor and dementia. Actually, keeping your blood vessels healthy might help protect your brain in the long run. There’s no evidence that Lipitor causes Alzheimer’s or serious memory problems, which eases a lot of patients’ minds.
Now, what about diabetes? High-dose statins can nudge blood sugar up, and yes, there’s a very small risk of new diabetes, especially if you’re already close to the line. But, if you’re at risk for heart troubles, the benefits of preventing a heart attack or stroke almost always outweigh the downside of a few points higher on your blood sugar check.
Wondering about dealing with grapefruit juice? Lipitor is one of the statins most likely to be affected by grapefruit, which can boost blood levels and raise side effect risk. Avoid large amounts of grapefruit or its juice unless your doctor says it’s okay. There are other meds and supplements that can interact with Lipitor, like certain antibiotics, antifungals, HIV medicines, and St. John’s wort. It’s always smart to check in at the pharmacy and keep a list on your phone of all the stuff you take.
Real talk: people sometimes get tired of taking Lipitor or any daily drug, especially if they don’t "feel" sick in the first place. But skipping pills or stopping suddenly rebounds your cholesterol to its old levels. For some folks, even higher. Building routines, using pill-minder apps, or linking your pill habit to another daily must-do is the number one tip for staying consistent. If you travel or juggle a crazy schedule, toss a strip of pills in your bag with your toothbrush.
There are other little ways to limit side effects. If you notice muscle aches, ask your doctor if you can drop your dose, change timing, or try taking coenzyme Q10—some people swear by it, though the science is still a bit soft. Want to keep your liver and muscles happy? Avoid super heavy drinking and steer clear of illegal or "street" drugs. Pat yourself on the back by moving more—exercise, even just walking, helps your "good" cholesterol and eases some side effects too.
Watch your wallet. Lipitor was a pricy blockbuster, but generic atorvastatin is dirt cheap these days—sometimes less than ten bucks for a month’s supply. There is no difference in effect between name brand and generic, so don’t let anyone tell you otherwise. If your insurance wants the generic, it’s absolutely fine to go with that.
Still skeptical or nervous? You’re not alone. People love to swap Lipitor stories, and Google doesn’t always help. But each person’s risk, benefit, and experience are different. If you’re worried about side effects, most can be spotted and solved fast, and your doctor can adjust your regimen as needed. The key takeaway: don’t skip doses or stop on your own—always check in with your provider about any worries. A single pill means a lot for your long-term heart and brain health.
Here’s one last tip to remember: Lipitor isn’t a free pass for all-you-can-eat buffets or dodging exercise. It’s part of the routine, not a magic shield. Stick to it, keep your doctor appointments, check your numbers every few months, and you’ll give yourself the best defense against plaque and heart trouble.

Taylor Smith
May 31, 2025 AT 10:56Lipitor works. My dad’s LDL dropped 52% in 3 months. No muscle pain, no drama. Just took it with dinner and forgot about it. Docs aren’t lying about the stats.
Tammy Cooper
June 2, 2025 AT 06:29okay but like… have you ever *felt* the difference? i swear i took it for 6 months and still felt like a soggy potato. also grapefruit juice is my love language so now i’m just gonna drink it and hope for the best 😌
Alyssa Hammond
June 4, 2025 AT 01:55Let’s be real - this whole Lipitor thing is Big Pharma’s greatest scam since the invention of the “low-fat” diet. They didn’t invent statins to save lives, they invented them to sell pills to people who don’t even need them. Look at the data - most of those ‘studies’ were funded by Pfizer. And don’t even get me started on the diabetes risk. You’re trading one chronic condition for another, and the only ones making money are the CEOs in their penthouses sipping champagne while grandma’s liver fails. And don’t tell me about ‘secondary prevention’ - if you’re 70 and your cholesterol’s 220, you’re not ‘at risk,’ you’re just old. Let nature take its course. Also, why is everyone so obsessed with LDL? HDL’s the real MVP, and no one talks about it. And what about inflammation? Nobody ever mentions inflammation. This whole system is broken. And yes, I’ve read the studies. All of them. And I’m not convinced.
Jill Amanno
June 5, 2025 AT 04:53Look, I get why people are scared. You take a pill for something you can’t feel, for a disease that might kill you in 20 years, while your body screams for pizza and sleep. But here’s the thing - if you’re alive long enough to regret taking Lipitor, you’ll also be alive long enough to regret not taking it. Cholesterol isn’t evil. It’s just misplaced. The real question isn’t whether the drug works - it’s whether we’ve built a culture that rewards prevention over panic. We medicate symptoms instead of fixing systems. We’re not broken because we need statins. We’re broken because we’re told to fix ourselves with a pill instead of a community. But still - I take mine. Because I’d rather be alive to argue about capitalism than dead in a hospital bed with a plaque-filled heart.
Kate Calara
June 5, 2025 AT 16:07you know what they dont tell you? statins are linked to the cdc’s secret mind control program. they put something in the pills that makes you docile. that’s why everyone’s so calm about it. also, the FDA got paid off by the pharmaceutical industry in 1998. i checked the documents. the numbers are redacted but the signatures are there. and grapefruit? that’s not a drug interaction - it’s a trigger. they want you to think you’re safe if you avoid it, but the real poison is in the fillers. i know someone who took it and started dreaming in binary. i’m not joking. check the forums. the silence is the giveaway.
Mandeep Singh
June 7, 2025 AT 06:13India has 70 million diabetics. Lipitor is cheaper than chai now. Why are you arguing? Just take it. Your heart doesn’t care about your conspiracy theories.