International Pharmacovigilance: How Global Drug Safety Monitoring Is Being Harmonized
 Jan, 5 2026
Jan, 5 2026
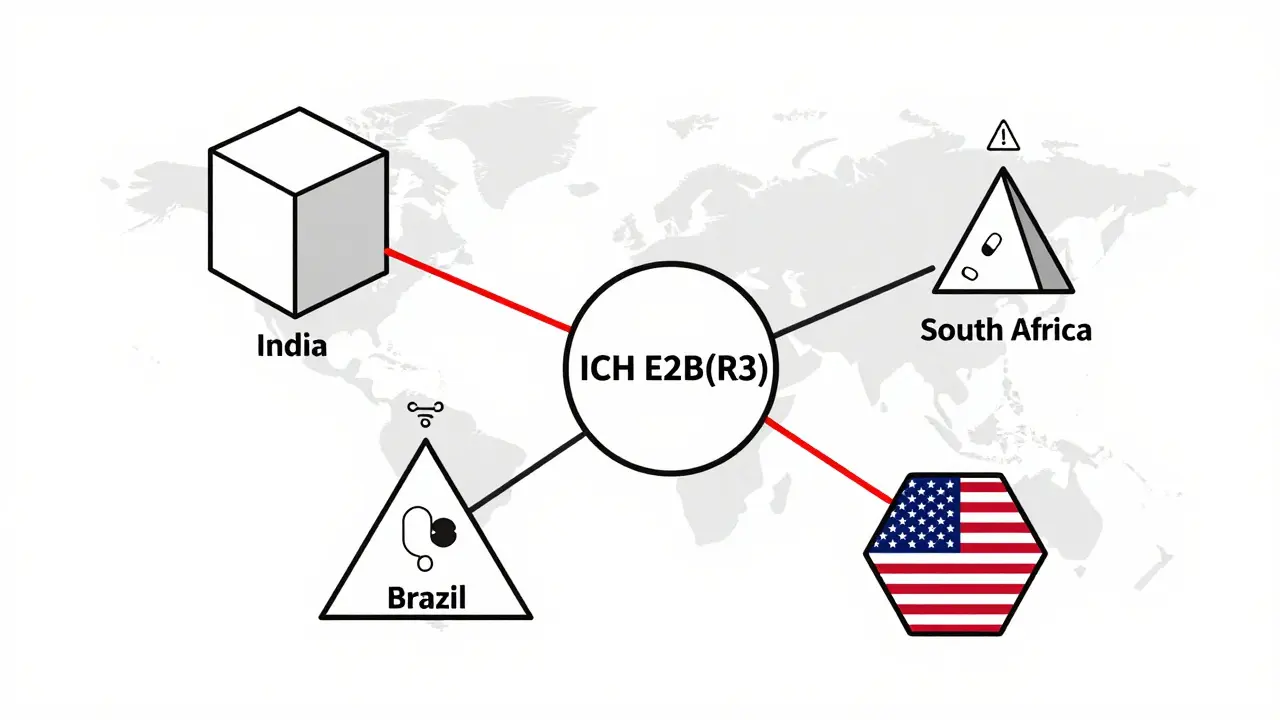
Every year, millions of people take generic drugs made in one country and used in another. But what happens when something goes wrong? A patient in Brazil has a rare reaction to a medicine made in India, prescribed in South Africa, and monitored by regulators in the U.S. Who tracks it? How fast do they respond? And why does it take so long for some countries to act?
The answer lies in pharmacovigilance harmonization-the global push to make drug safety monitoring consistent across borders. It’s not just about paperwork. It’s about saving lives. When safety systems don’t talk to each other, dangerous signals get lost. When reporting rules change from country to country, companies waste months reformatting reports. And when low-income nations can’t afford the tech to detect side effects, patients pay the price.
How Global Drug Safety Rules Got Started
The modern system began in 1990, when regulators from the U.S., Europe, and Japan came together to form the International Council for Harmonisation (ICH). Their goal? Stop duplicating efforts. Before ICH, a single drug could require six different safety reports just to enter three markets. Companies spent more time adjusting formats than studying safety data.
ICH didn’t create new rules-it aligned them. The result? The ICH E2 series. E2B(R3) became the global standard for electronic adverse event reporting. E2E defined how companies must plan for risks before a drug even hits shelves. And PSURs (Periodic Safety Update Reports) now follow the same structure whether they’re sent to the FDA, EMA, or Health Canada.
Today, 95% of pharmaceutical companies in the U.S. and EU follow these guidelines. But that’s not the whole story. In 2024, only 42% of companies in emerging markets had fully adopted ICH E2B(R3). The gap isn’t just technical-it’s financial. Setting up a compliant system costs $2-$5 million for a mid-sized firm. Many can’t afford it.
Where the Rules Still Don’t Match Up
Even with ICH, differences remain. Take the 15-day rule. The FDA requires urgent reporting of serious, unexpected side effects within 15 calendar days. The EMA? It depends. For some drugs, it’s 7 days. For others, it’s 30. And Japan’s PMDA doesn’t even count weekends.
Then there’s risk management. The EU forces every new drug to have a full Risk Management Plan (RMP). The U.S. only requires it for high-risk drugs-about 1.2% of all approved medicines. That means a company might spend months building a detailed safety plan for Europe, only to submit a bare-bones version to the FDA.
One pharmacovigilance manager in London told me last year: “I spend 35-40% of my time just rewriting the same report for different regions.” That’s not efficiency. That’s waste.
And it’s not just paperwork. Definitions vary. What’s “unexpected” in Germany might be “expected” in Canada. A 2021 CIOMS report found a 47% inconsistency rate in how companies label adverse events across regions. That leads to missed signals-and delayed recalls.
Technology Is Bridging the Gaps
AI is changing the game. Since 2022, the EMA and FDA have used machine learning to scan millions of reports. The results? Signal detection is 30-40% faster. Japan’s PMDA cut false alarms by 25% using AI models trained on 12 million patient records.
Real-world data (RWD) is another game-changer. The EU now pulls safety signals from electronic health records. The FDA’s Sentinel Initiative tracks 300 million U.S. patients. DARWIN EU, the EMA’s system, covers 100 million across seven countries.
But here’s the problem: Brazil and South Africa can’t process more than 15% of their potential RWD. Why? No digital health records. No data infrastructure. No funding.
That’s why WHO’s Global Smart Pharmacovigilance Strategy-drafted in October 2024-is so critical. It aims to set common data standards for all 150 member countries by 2027. If it works, a pharmacist in Nairobi could flag a dangerous reaction, and the system would alert regulators in Tokyo and Toronto within days.

Who’s Doing It Right-and Who’s Falling Behind
Look at Canada. Their Vigilance Program follows ICH closely but still requires 30-day reporting for serious events. It’s not perfect, but it’s consistent. Novartis, after building a single global safety database, cut duplicate case entry by 92%. They found critical safety signals 38 days faster.
China’s NMPA has improved fast since 2020. But they still require local reporting within 15 days-forcing multinational companies to submit the same data twice: once for China, once for ICH.
Meanwhile, the world’s largest safety database-VigiBase, run by WHO-holds over 35 million individual case reports from 134 countries. It’s a treasure trove. But only 31% of low- and middle-income countries have fully implemented the ICH E2B(R3) standard needed to feed into it.
The data doesn’t lie: 74% of pharmacovigilance staff in poorer nations say they lack resources to even meet basic standards. In high-income countries? Only 8% say the same.
The Human Cost of Misalignment
This isn’t abstract. In 2023, a liver toxicity signal from a generic antibiotic was detected in Germany but missed in Nigeria because the local system couldn’t process electronic reports. By the time it was flagged in Lagos, 17 patients had been hospitalized. One died.
Deloitte estimates that full harmonization could prevent 1,200-1,500 drug-related deaths per year. That’s not a number. That’s families. That’s mothers, fathers, children.
And the cost of inaction? $2.3 billion a year in wasted resources. Plus, an extra $1.8 billion needed just to bring basic systems up to speed in low-income countries.

What’s Next? The Road to True Global Safety
ICH announced in March 2024 that it’s working on harmonizing AI validation standards-something no one has done before. By mid-2026, companies might finally have one set of rules for how to train and test their safety algorithms.
The FDA, EMA, and PMDA formed a joint task force in January 2024. They’ve already aligned 78% of their risk plan requirements for new biologics. That’s progress.
But true harmony isn’t just about tech or templates. It’s about equity. A drug safety system that works for Pfizer but not for a clinic in rural Kenya isn’t a system-it’s a privilege.
That’s why the future of pharmacovigilance isn’t just about faster reporting or smarter AI. It’s about funding. Training. Infrastructure. Supporting local regulators in places like Ghana, Bangladesh, and Peru so they can participate, not just receive.
The tools exist. The guidelines are there. What’s missing is the will to make them work for everyone.
What You Need to Know
- ICH E2B(R3) is the global standard for electronic adverse event reporting-adopted by 89% of top pharma companies.
- The FDA and EMA have different deadlines for urgent reports: 15 days vs. variable timelines based on drug type.
- AI is cutting signal detection time by 30-40% in advanced markets but is out of reach for most low-income countries.
- VigiBase, WHO’s global database, holds over 35 million reports-but only 31% of emerging markets can feed into it properly.
- Companies spend 22% more on pharmacovigilance due to regulatory fragmentation.
- By 2027, WHO aims to establish common data standards across 150 countries.
What is pharmacovigilance harmonization?
Pharmacovigilance harmonization is the process of aligning drug safety monitoring rules, formats, and technologies across countries so that adverse event data can be shared, compared, and acted on quickly and consistently. It’s led by organizations like the ICH and WHO to prevent duplication, speed up detection of dangerous side effects, and improve global patient safety.
Why do different countries have different safety reporting rules?
Each country has its own regulatory history, resources, and priorities. The U.S. focuses on high-risk drugs, while the EU requires safety plans for all new medicines. Some nations lack the infrastructure to collect real-world data or process electronic reports. These differences aren’t random-they’re shaped by funding, political systems, and healthcare access.
How does AI help with global drug safety?
AI scans millions of adverse event reports to spot unusual patterns faster than humans. The EMA and FDA now use AI to cut signal detection time by 30-40%. Japan’s system reduced false alarms by 25%. But AI tools need clean, standardized data-and many countries still rely on paper forms or outdated systems.
What’s the biggest barrier to global pharmacovigilance?
The biggest barrier is inequality. High-income countries have digital health records, AI tools, and trained staff. Low- and middle-income countries often lack funding, internet access, and regulatory capacity. Without investment in their systems, global safety remains incomplete.
Can generic drugs be monitored as effectively as brand-name ones?
Yes-but only if the systems are aligned. Generic drugs are often made in one country and sold in many. If reporting rules vary, side effects from the same batch may go unnoticed in some regions. Harmonization ensures that a safety signal from a generic drug in India is seen and acted on in Canada, Brazil, or South Africa.
What should patients know about international pharmacovigilance?
If you take a generic medicine, your safety is tied to global systems. A side effect you report might help protect someone halfway across the world. But those systems only work if they’re strong everywhere. Support policies that fund global drug safety infrastructure-it’s not charity. It’s public health.

Susan Arlene
January 5, 2026 AT 22:31Mukesh Pareek
January 6, 2026 AT 07:51Jeane Hendrix
January 7, 2026 AT 00:23Rachel Wermager
January 7, 2026 AT 23:33Joann Absi
January 8, 2026 AT 16:20Tom Swinton
January 10, 2026 AT 07:55Leonard Shit
January 11, 2026 AT 03:17Wesley Pereira
January 12, 2026 AT 12:50Isaac Jules
January 14, 2026 AT 08:18Ashley S
January 15, 2026 AT 15:05Stuart Shield
January 16, 2026 AT 19:31Pavan Vora
January 17, 2026 AT 13:21Indra Triawan
January 18, 2026 AT 17:45Susan Arlene
January 19, 2026 AT 20:49