IBS Diet Guide: FODMAP, Low-Residue, and Elimination Plans Explained
 Nov, 19 2025
Nov, 19 2025
If you live with irritable bowel syndrome (IBS), you’ve probably tried dozens of diets. Maybe you cut out dairy. Maybe you went gluten-free. Maybe you ate nothing but rice and chicken for weeks-and still felt bloated. The truth? Not all IBS diets are created equal. Three approaches dominate clinical practice today: low-FODMAP, low-residue, and elimination diets. Each has different rules, different goals, and very different results.
What Is the Low-FODMAP Diet, and Why Does It Work?
The low-FODMAP diet isn’t just another “eat clean” trend. It’s a scientifically backed, three-phase system developed at Monash University in Melbourne to target specific carbohydrates that ferment in your gut and trigger IBS symptoms. FODMAP stands for Fermentable Oligo-, Di-, Mono-saccharides And Polyols. These are sugars like fructose, lactose, and sugar alcohols (sorbitol, mannitol) that some people can’t absorb well. When they reach the colon, bacteria feast on them-and produce gas, bloating, pain, and diarrhea.
The diet has three clear phases:
- Elimination (2-6 weeks): You cut out all high-FODMAP foods. That means no onions, garlic, apples, wheat, honey, milk, beans, or artificial sweeteners like xylitol. You eat only foods verified as low-FODMAP by Monash’s lab testing-portions matter. A teaspoon of garlic is okay. Two? Not anymore.
- Reintroduction (8-12 weeks): You slowly add back one FODMAP group at a time. Start with fructans (wheat, onions). Eat 3 grams of it in one meal. Wait 3 days. Track symptoms. Then try galacto-oligosaccharides (beans, lentils). Then lactose. Then excess fructose. Then polyols. This phase tells you exactly which triggers are yours.
- Personalization (lifetime): Most people can eat 50-80% of the foods they eliminated. You don’t need to avoid garlic forever. You just need to know that 1 clove is fine, but 3 is not.
Studies show 75-80% of IBS patients see major improvement in bloating, pain, and bowel habits. That’s not magic. It’s precision. The Monash FODMAP app, used by over 2 million people, lets you scan barcodes and check serving sizes in real time. It’s the closest thing to a food GPS for IBS.
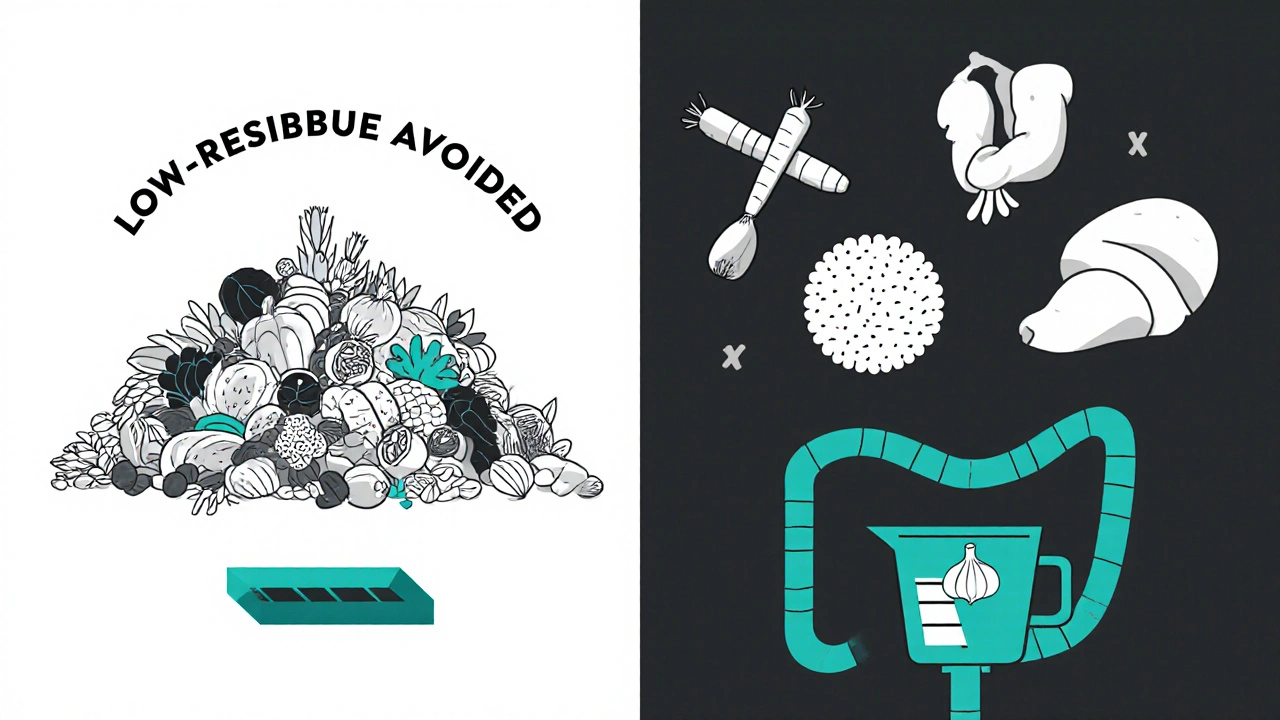
Low-Residue Diet: When Less Fiber Actually Helps
The low-residue diet is older and simpler. It’s not designed for long-term IBS management-it’s meant for short-term relief, especially when your gut is inflamed or you’re preparing for a colonoscopy. It cuts fiber to 10-15 grams per day (normal intake is 25-38 grams). You avoid:
- Raw fruits and vegetables
- Whole grains
- Nuts, seeds, and popcorn
- Legumes
- High-fiber cereals
You eat white bread, white rice, cooked carrots, lean meats, eggs, and lactose-free dairy. The goal? Reduce stool volume and frequency. It works best for people with diarrhea-predominant IBS (IBS-D). One study found 45% of IBS-D patients had fewer bowel movements on this diet, compared to 75% on low-FODMAP.
But here’s the catch: low-residue diets are nutritionally risky. Cutting out fiber, fruits, and whole grains for more than a few weeks can drop your folate intake by 35% and calcium by 25%. It’s also useless-and even harmful-for constipation-predominant IBS (IBS-C). If you’re struggling to go, this diet will make it worse.
Most gastroenterologists now reserve this diet for flare-ups or medical procedures, not as a long-term IBS solution. It’s a band-aid, not a cure.
General Elimination Diets: The Wild West of IBS Eating
Elimination diets sound simple: remove common trigger foods for 2-4 weeks, then add them back one by one. Common suspects? Dairy, gluten, caffeine, eggs, soy, corn, citrus. But unlike the low-FODMAP diet, there’s no standard protocol. No lab-tested portion sizes. No science-backed challenge doses.
That’s why results are inconsistent. Only about 30-50% of people find their real triggers this way. Many think they’re sensitive to gluten-but it’s actually fructans in wheat. Or they blame dairy, but it’s lactose, not casein. Without knowing the difference, you’re guessing.
Elimination diets are easier to start. You don’t need an app. You don’t need to weigh your food. But they’re harder to interpret. A 2023 study from the University of Virginia found that 35% of people who tried this method skipped the reintroduction phase entirely-and gave up, thinking the diet didn’t work.
They’re useful if you can’t access a FODMAP-trained dietitian. But they’re not as accurate. And if you cut out too many foods without guidance, you risk nutrient gaps or disordered eating patterns.
Which Diet Is Right for You?
Let’s break it down:
| Feature | Low-FODMAP | Low-Residue | General Elimination |
|---|---|---|---|
| Primary Goal | Identify specific carbohydrate triggers | Reduce stool volume | Find food sensitivities |
| Best For | Bloating, pain, mixed IBS | Diarrhea-predominant IBS (short-term) | Resource-limited settings |
| Duration | 3-6 months (full protocol) | 2-4 weeks max | 4-6 weeks |
| Success Rate | 75-80% | 40-45% | 40-50% |
| Nutrition Risk | Moderate (if not reintroduced) | High (fiber, vitamins) | Moderate (if too many foods cut) |
| Complexity | High (requires tracking, app) | Low | Medium |
For most people with IBS, the low-FODMAP diet is the best starting point. It’s the only one backed by over 20 randomized trials and endorsed by the American College of Gastroenterology. But it’s not for everyone.
If you have severe diarrhea and need quick relief, a short low-residue phase might help. If you’re in a rural area with no dietitian access, a basic elimination diet is better than doing nothing. But if you want to eat normally again-without constant fear of food-the FODMAP approach is the only one that gives you back control.
What You Need to Succeed
Doing this right takes tools and support:
- Monash FODMAP App: The gold standard. $9.99/month or $49.99/year. Scans barcodes, lists safe portions, and has a symptom tracker.
- Food Scale: Weighing portions matters. A “low-FODMAP” apple is okay at 1/2 cup sliced. Two cups? High-FODMAP.
- Symptom Journal: Write down what you ate, when, and how you felt. Look for patterns.
- Professional Guidance: A registered dietitian trained in FODMAPs cuts your failure rate in half. Look for Monash-certified providers-they’re listed on their website.
Most people struggle most during reintroduction. That’s when symptoms flare up again-and panic sets in. But that’s the point. If you feel bloated after eating 10 grams of polyols (like in sugar-free gum), you now know: polyols are your trigger. You don’t need to avoid them forever. Just avoid them in large amounts.
Common Mistakes (And How to Avoid Them)
Here’s what goes wrong-and how to fix it:
- Mistake: Skipping the reintroduction phase. Fix: Even if you feel better, don’t stop. You’re missing the chance to eat more foods.
- Mistake: Cutting out too many foods at once. Fix: Only eliminate high-FODMAP foods in Phase 1. Don’t go gluten-free or dairy-free unless you’re testing those specifically.
- Mistake: Trusting “low-FODMAP” labels on packaged food. Fix: Check ingredients. Inulin, chicory root, honey, agave, and high-fructose corn syrup are hidden FODMAPs.
- Mistake: Eating out without planning. Fix: Use Monash’s “FODMAP Friendly” restaurant cards. Ask for plain grilled meat, steamed veggies (carrots, zucchini), and rice.
One patient from Melbourne told me: “I thought I had to give up all my favorite foods. Turns out, I just had to give up the wrong portions. Now I eat pasta, garlic bread, and strawberries-with limits.”

Who Shouldn’t Try This?
The low-FODMAP diet isn’t safe for everyone:
- People with eating disorders: Restrictive diets can trigger relapse. 15% of IBS patients have a history of disordered eating.
- Those with severe malnutrition: Cutting out whole food groups without supervision can worsen deficiencies.
- People with IBS-C who need fiber: Low-FODMAP is still low-fiber. If you’re constipated, you may need soluble fiber like psyllium, not more restriction.
If you’re unsure, talk to a doctor or dietitian first. This isn’t a DIY diet. It’s a medical tool.
What’s Next for IBS Diets?
Science is moving fast. Monash’s new app version (5.2, released September 2023) uses AI to suggest meals based on your symptoms. Researchers are testing whether gut bacteria can predict who will respond to FODMAP restriction. A major NIH trial is underway to find biomarkers for FODMAP sensitivity.
But the core message hasn’t changed: IBS isn’t caused by one food. It’s caused by how your gut reacts to certain carbs. And with the right plan, you don’t have to live with constant pain.
Most people find freedom-not restriction-after the reintroduction phase. You’re not giving up food. You’re learning how to eat it again.
Can I do the low-FODMAP diet without an app?
You can, but it’s much harder. The Monash FODMAP app is the only tool with lab-tested portion sizes for over 1,200 foods. Without it, you risk eating too much of a “low-FODMAP” food and triggering symptoms. Free lists exist online, but they’re outdated and don’t account for serving size. If you can’t afford the app, ask your dietitian for printed guides or check your local library-they often have copies.
How long does it take to see results on low-FODMAP?
Most people notice improvement within 2-6 weeks during the elimination phase. Some feel better in just 3-5 days, especially with bloating and diarrhea. But full symptom relief often takes longer. Don’t rush the reintroduction phase-this is where you learn your personal triggers. Patience here saves you from lifelong unnecessary restrictions.
Will I lose weight on a low-FODMAP diet?
Some people do, but it’s not the goal. Weight loss happens because you’re cutting out high-calorie, processed foods like bread, pastries, and sugary snacks. If you’re losing weight unintentionally or feeling weak, you’re not eating enough. Focus on low-FODMAP proteins (eggs, chicken, tofu), healthy fats (olive oil, nuts in small amounts), and safe carbs (rice, oats, potatoes). Talk to a dietitian if you’re losing more than 1-2 kg per week.
Can I drink alcohol on low-FODMAP?
Some types are okay in moderation. Clear spirits like vodka, gin, and tequila (without mixers) are low-FODMAP. Dry wines (white, red) are usually fine in 150ml servings. Avoid beer (barley), sweet wines (high fructose), and cocktails with honey, agave, or fruit juice. Mixers like tonic water (high in sugar alcohols) can trigger symptoms. Always check the Monash app before drinking.
What if the low-FODMAP diet doesn’t work for me?
About 20-25% of people don’t improve, even when done perfectly. That doesn’t mean you’re broken-it means your IBS might be triggered by something else: stress, bile acid malabsorption, small intestinal bacterial overgrowth (SIBO), or even food intolerances outside FODMAPs. Talk to your doctor about further testing. You might need a different approach, like a bile acid binder, peppermint oil, or gut-directed hypnotherapy. Don’t give up-just pivot.
Final Thoughts
IBS isn’t caused by bad food. It’s caused by how your gut responds to certain foods. The low-FODMAP diet isn’t about restriction-it’s about discovery. It gives you back the power to eat without fear. The low-residue diet is a temporary tool. General elimination diets are a shot in the dark. Only FODMAP gives you a map.
You don’t have to live with bloating, pain, or constant bathroom trips. With the right plan, you can eat pasta, garlic, apples, and beans-just not all at once, and not in huge amounts. The goal isn’t to eat perfectly. It’s to eat freely, without anxiety.
Start with the elimination phase. Track everything. Use the app. See a dietitian if you can. And remember: this isn’t forever. It’s a path back to your favorite foods-not away from them.

Nick Naylor
November 21, 2025 AT 14:50The low-FODMAP diet is the only scientifically valid approach here-period. The rest are anecdotal garbage masquerading as nutrition. You want to know why 75-80% of patients improve? Because it’s not a fad-it’s a biochemistry protocol. The Monash app isn’t a luxury; it’s a clinical necessity. Anyone who says they ‘don’t need it’ is either lying or dangerously misinformed. And don’t get me started on ‘general elimination diets’-that’s just culinary guesswork with a side of malnutrition. If you’re not tracking portions to the gram, you’re not doing it right.
Brianna Groleau
November 21, 2025 AT 19:20I just want to say how deeply this resonated with me. I spent three years cycling through every diet under the sun-keto, paleo, vegan, gluten-free, dairy-free-and still woke up every morning feeling like my insides were staging a rebellion. When I finally found the FODMAP protocol with a dietitian, it didn’t feel like restriction-it felt like liberation. I can eat garlic now. Not a whole bulb. Just one clove. And that one clove? It’s the difference between living and just existing. I cried the first time I ate a slice of sourdough without panicking. This isn’t just food science-it’s emotional healing.
Rusty Thomas
November 23, 2025 AT 06:49Okay but have you seen what’s in the Monash app? Like, it’s basically a cult. I swear they’re tracking your bowel movements through your phone’s camera. And why is it $50 a year? That’s a whole month’s rent for some people. Also-what if your gut hates ALL FODMAPs? What then? Are you just gonna live on boiled chicken and rice forever? I think Big Pharma is behind this. They want you dependent on apps and dietitians so you never get better. Just saying.
Sarah Swiatek
November 23, 2025 AT 21:19Let’s be real: the low-FODMAP diet is the only thing that actually works-but most people fail at phase two. Not because they can’t stick to it, but because they’re terrified of the symptoms returning. I’ve seen so many people quit reintroduction because they felt bloated after eating a single apple slice-and immediately went back to the elimination phase, convinced they’d failed. But that’s not failure. That’s data. You’re not supposed to feel great every time you reintroduce. You’re supposed to learn what your threshold is. One person’s trigger is another’s snack. It’s not about perfection. It’s about personalization. And yes, it’s exhausting. But so is living with constant pain. Sometimes, the hardest path is the only one that leads home.
Dave Wooldridge
November 25, 2025 AT 10:37They don’t want you to know this-but FODMAPs are a government ploy to control your gut. The Monash app? Owned by the WHO. The ‘science’? Fabricated by Big Ag to sell more supplements. They’re pushing this because they know if you eat real food-like onions and garlic-you won’t need their drugs. That’s why they make it sound so complicated. You need an app, a scale, a dietitian, a journal… it’s designed to make you feel powerless. Meanwhile, real people have healed with just water, salt, and willpower. Stop trusting the system. Start trusting your body.
Rebecca Cosenza
November 25, 2025 AT 21:36Low-residue for diarrhea? Sure. But don’t act like it’s a cure. You’re just starving your microbiome. You think you’re helping? You’re just delaying the inevitable. And if you’re cutting out fiber because you’re scared of bloating? That’s not health. That’s fear. You’re not fixing your gut-you’re silencing it. And silence isn’t peace. It’s surrender.
Lemmy Coco
November 27, 2025 AT 02:21hey i tried the fodmap thing but i kept mixing up the portions like i thought 1/2 cup of apples was okay but turns out it was like 3/4? and then i got bloated and gave up. also i forgot to write down my symptoms and now i dont even remember what made me feel bad. maybe i should just eat rice forever idk. sorry for the typos lol
rob lafata
November 28, 2025 AT 07:31You people are adorable. You think this is about food? It’s about control. The low-FODMAP diet isn’t a treatment-it’s a behavioral prison. You’re not learning to eat-you’re learning to obey. You scan barcodes like trained dogs. You weigh your strawberries. You avoid garlic like it’s poison. And you call it ‘freedom’? That’s not healing. That’s obedience training wrapped in a $50 app subscription. The real problem? You’re not listening to your body-you’re listening to a spreadsheet. And the moment you stop trusting your own gut-literally-you become a product. Not a patient. A consumer. And that’s the real tragedy.