How Testosterone Levels Influence BPH Symptoms: What Men Need to Know
 Oct, 12 2025
Oct, 12 2025
Key Takeaways
- BPH (Benign Prostatic Hyperplasia) is linked to hormonal shifts, especially changes in testosterone levels.
- Both high and low testosterone can affect prostate growth, but the relationship is not a simple cause‑and‑effect.
- Accurate hormone testing, PSA monitoring, and symptom scoring help clinicians tailor treatment.
- Lifestyle factors-weight, exercise, diet, and sleep-moderately influence hormone balance and BPH severity.
- When testosterone therapy is considered, urologists weigh BPH risk against benefits for mood, libido, and muscle mass.
Understanding BPH and Its Symptoms
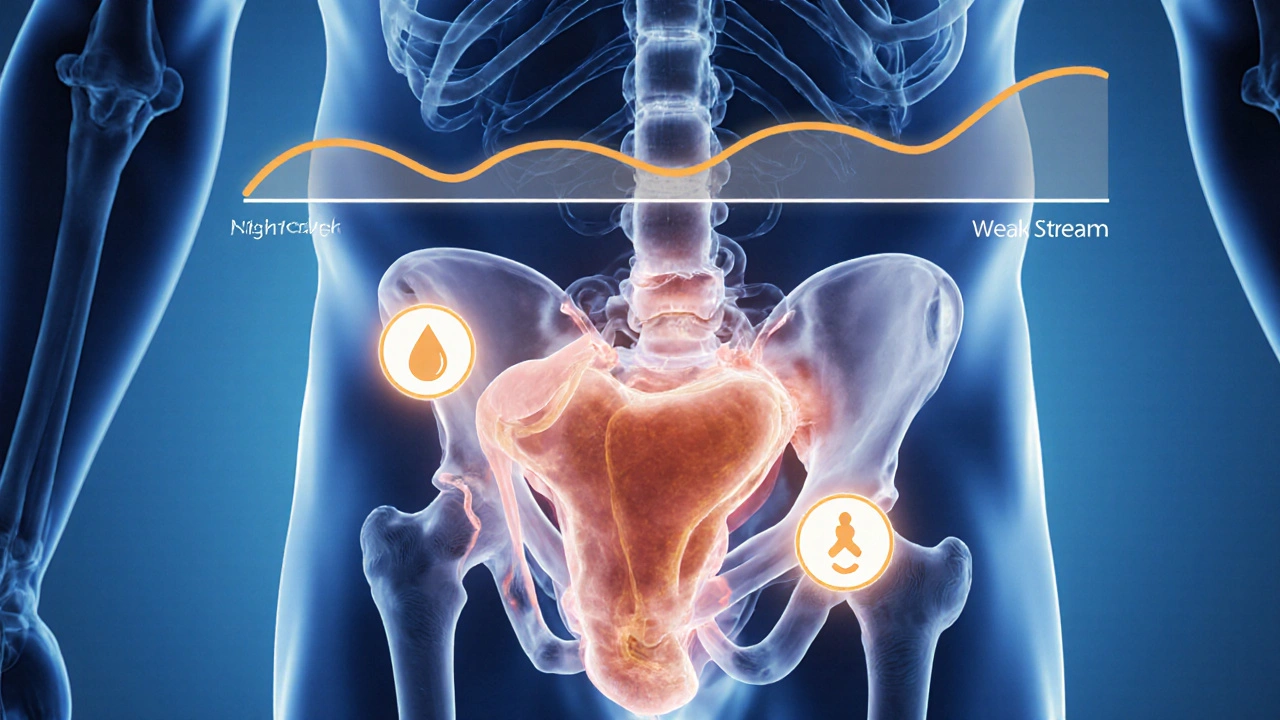
When doctors talk about BPH is a non‑cancerous enlargement of the prostate gland that often causes urinary symptoms such as frequent urination, weak stream, and nighttime trips to the bathroom, they’re describing a condition that affects roughly 30% of men aged 50 and climbs to 70% by age 80. The prostate sits just below the bladder, and any increase in its size squeezes the urethra, making it harder for urine to flow.
Clinicians usually grade symptoms with the International Prostate Symptom Score (IPSS). A score of 0-7 is mild, 8-19 moderate, and 20-35 severe. Knowing the score helps decide whether medication, minimally invasive procedures, or surgery is needed.
What Testosterone Is and How Levels Vary
Testosterone is the primary male sex hormone, produced mainly in the Leydig cells of the testes and, to a lesser extent, in the adrenal glands. Normal serum ranges for adult men are roughly 300-1,000ng/dL, but levels naturally decline about 1% per year after the age of 30.
Factors that push testosterone up or down include age, obesity, chronic illness, medication (especially steroids or opioids), and lifestyle choices like sleep quality and resistance training.
How Testosterone Interacts With the Prostate
The prostate relies on androgens-testosterone and its more potent derivative dihydrotestosterone (DHT)-to maintain tissue health. Inside the gland, the enzyme 5‑alpha‑reductase converts testosterone into DHT, which binds androgen receptors with higher affinity.
DHT is a potent androgen that drives prostate cell proliferation and can exacerbate BPH growth. Because only a fraction of circulating testosterone becomes DHT, the absolute blood testosterone level does not perfectly predict prostate exposure.
Research suggests that low testosterone may trigger a compensatory rise in 5‑alpha‑reductase activity, unintentionally increasing DHT locally. Conversely, very high testosterone can saturate the enzyme system, also boosting DHT. The net effect is a U‑shaped curve: both extremes may favor prostate enlargement.

Research Findings on Testosterone Levels and BPH Symptoms
Large cohort studies from the US, Europe, and Asia provide mixed signals:
- A 2022 longitudinal analysis of 7,400 men (mean age 58) found that men in the highest quintile of total testosterone had a 12% higher odds of moderate‑to‑severe IPSS scores compared with those in the middle quintile.
- A 2021 meta‑analysis of 15 randomized trials involving testosterone replacement therapy (TRT) reported no significant increase in prostate volume over 12months, but a modest rise in urinary frequency was noted in 8% of participants.
- Conversely, a 2023 Korean study highlighted that men with low free testosterone (<6pg/mL) showed a 17% increase in PSA and a higher rate of nocturia, suggesting that insufficient androgen activity can also aggravate symptoms.
Overall, the data point to a nuanced relationship: hormone balance matters more than absolute numbers. Clinicians now use a “hormonal health window”-typically 400-600ng/dL for total testosterone-to stay within a range where BPH risk does not spike.
Testing and Interpreting Hormone Levels
When a man presents with urinary complaints, a urologist may order three key labs:
- Total testosterone (ng/dL) - reflects overall production.
- Free testosterone (pg/mL) - the biologically active fraction not bound to SHBG.
- PSA (ng/mL) - helps rule out prostate cancer and monitors glandular activity.
Interpretation tips:
- If total testosterone <300ng/dL AND PSA is rising, consider a low‑testosterone‑related BPH flare.
- If testosterone >900ng/dL with a high IPSS, evaluate for exogenous androgen use or anabolic steroid exposure.
- Free testosterone <5pg/mL often signals a need for lifestyle or medical intervention, even when total testosterone appears normal.
Repeat testing after a 6‑week lifestyle intervention can clarify whether the hormone shift is transient.
Managing BPH When Testosterone Is High or Low
Therapeutic choices hinge on hormone status and symptom severity.
- Alpha‑blockers (e.g., tamsulosin): Relax prostate smooth muscle, improve flow regardless of testosterone.
- 5‑alpha‑reductase inhibitors (e.g., finasteride, dutasteride): Lower DHT, shrink gland size over 6-12months-especially useful when testosterone is high.
- Testosterone Replacement Therapy (TRT): For men with clinically low testosterone and bothersome BPH, start with a low dose and monitor IPSS and PSA every 3 months.
- Combination therapy: Alpha‑blocker + 5‑alpha‑reductase inhibitor can address both dynamic and static components of obstruction.
When considering TRT, a urologist will often target the mid‑range hormonal window and may prescribe a 5‑alpha‑reductase inhibitor concurrently to keep DHT in check.

Lifestyle Tips That Influence Hormones and Prostate Health
Small daily habits can shift the hormonal curve enough to ease BPH symptoms.
- Weight management: Every 5% increase in body fat is linked to a ~1% rise in estrogen and a modest drop in free testosterone.
- Resistance training: 3-4 sessions per week can boost total testosterone by 10‑15% in men over 40.
- Sleep hygiene: Less than 6hours of REM sleep cuts nighttime testosterone peaks by up to 30%.
- Dietary choices: Foods rich in zinc (oysters, pumpkin seeds) and vitamin D support testosterone synthesis; limiting excessive soy or flaxseed, which contain phytoestrogens, may help men sensitive to estrogenic effects.
- Limit alcohol and nicotine: Chronic heavy drinking can depress Leydig cell function; smoking is associated with higher DHT activity.
Adopting these habits alongside medical therapy often reduces the need for surgical intervention.
Frequently Asked Questions
Can low testosterone cause BPH?
Low testosterone can lead to a relative increase in DHT activity within the prostate, potentially aggravating urinary symptoms. However, the effect is usually milder than that seen with high testosterone or exogenous androgen use.
Is testosterone replacement therapy safe for men with BPH?
TRT can be safe if the patient’s baseline PSA is normal, IPSS is low‑to‑moderate, and hormone levels are kept within the 400-600ng/dL window. Regular monitoring every 3‑6months is essential to catch any worsening of symptoms.
Do 5‑alpha‑reductase inhibitors affect testosterone levels?
These drugs primarily block the conversion of testosterone to DHT, so total testosterone may rise slightly, but the change is usually not clinically significant. The main benefit is a reduction in prostate volume and symptom relief.
What PSA level should trigger a prostate specialist referral?
A PSA above 4ng/mL in men over 50, or a rapid rise of >0.75ng/mL per year, warrants further evaluation. Even with normal PSA, a high IPSS may prompt a urology consult.
Comparison of Testosterone Level Ranges and Associated BPH Risk
| Testosterone Range (ng/dL) | Typical Free Testosterone | Impact on DHT Production | Observed BPH Symptom Trend |
|---|---|---|---|
| 300-400 | Low (≤5pg/mL) | Compensatory ↑ 5‑α‑reductase activity | Modest increase in nocturia and weak stream |
| 401-600 | Optimal (5‑10pg/mL) | Balanced conversion | Stable symptoms; lowest risk of progression |
| 601-900 | High (≥10pg/mL) | ↑ substrate → ↑ DHT | Higher IPSS scores, especially in men >65 |
| >900 (often exogenous) | Very high | Marked ↑ DHT, possible saturation | Significant urinary obstruction risk |
Keeping testosterone within the middle window-while addressing lifestyle factors-offers the best chance of minimizing BPH flare‑ups.

Stephanie Zuidervliet
October 12, 2025 AT 16:24Wow!!! Another sooo detailed piece on testosterone and BPH-so many buzzwords!!! But where's the real talk about side‑effects???
Olivia Crowe
October 23, 2025 AT 09:32It's refreshing to see this balanced view-knowledge is power, and we can take charge of our health!
Aayush Shastri
November 3, 2025 AT 01:41In many South Asian families, discussions about testosterone therapy are still shrouded in stigma, yet the data we see here cuts through the myth. The article nicely outlines how both low and high levels can tip the prostate balance, which is valuable for men hesitant to seek help. I appreciate the inclusion of lifestyle factors; regular resistance training and proper sleep are universal, not just Western luxuries. Moreover, the nuance about DHT conversion resonates with what we observe in clinical practice back home. While the U‑shaped curve might sound academic, it mirrors real‑world cases where men on steroids experience sudden urinary urgency. Overall, this piece bridges the gap between research and everyday reality for a diverse audience.
Quinn S.
November 13, 2025 AT 18:50While the article is ostensibly comprehensive, it suffers from a lamentable lack of statistical rigor. The cited studies are mentioned without proper citation format, and the alleged “U‑shaped curve” is presented without accompanying confidence intervals. Such omissions undermine the credibility of any practitioner relying on this synthesis. A more scrupulous author would have provided raw data tables rather than vague percentages.
Dilip Parmanand
November 24, 2025 AT 11:58I get where you’re coming from-clarity is key, and the article could definitely sharpen its data presentation.
Sarah Seddon
December 5, 2025 AT 05:07Bravo on weaving science with storytelling! The way you paint the hormone dance feels like a vivid mural, making complex pathways feel alive. Readers will walk away both informed and inspired.
Ari Kusumo Wibowo
December 15, 2025 AT 22:15Look, we all want the truth without the drama-so kudos for keeping it real, but let’s not throw the baby out with the bathwater.
Hannah Gorman
December 26, 2025 AT 15:24The prevailing narrative that testosterone levels are the principal puppeteer behind BPH growth is, in my estimation, an over‑simplification that betrays a superficial grasp of endocrinology.
First, the article neglects to acknowledge the intricate feedback loops involving estrogen, prolactin, and inflammatory cytokines that also modulate prostatic tissue.
Second, the reliance on cross‑sectional data without longitudinal follow‑up renders any causal inference tenuous at best.
Third, the cited Korean study is presented without a critical appraisal of its sample size limitations, which undermines its purported significance.
Moreover, the discussion of DHT conversion glosses over the genetic polymorphisms in the SRD5A2 gene that can dramatically alter enzymatic activity.
Patients with the TT genotype, for example, may experience markedly higher intraprostatic DHT despite normal serum testosterone, a nuance absent from the overview.
The lifestyle recommendations, while well‑intentioned, conflate correlation with causation by implying that weight loss will unequivocally normalize hormone levels.
Numerous randomized trials have demonstrated that exercise improves insulin sensitivity without necessarily impacting circulating testosterone.
Additionally, the article fails to distinguish between total testosterone and bioavailable fractions, a distinction that is clinically paramount.
Free testosterone, measured via equilibrium dialysis, can diverge substantially from total levels, especially in men with altered SHBG concentrations.
The omission of SHBG dynamics is a glaring oversight that could mislead clinicians who rely on these biomarkers for therapeutic decisions.
When the authors refer to the “U‑shaped curve,” they do not provide the underlying statistical model, confidence intervals, or potential confounders.
Without this information, readers are left to accept a narrative that may be more speculative than evidentiary.
Furthermore, the brief mention of testosterone replacement therapy (TRT) omits discussion of the heterogeneity among formulations-gels, injections, and pellets each bear distinct risk profiles.
In particular, the risk of urinary frequency appears more pronounced with gel formulations, a point that warrants explicit acknowledgment.
In sum, while the article serves as a cursory primer, it stops far short of the rigorous analysis required for informed clinical practice.
Tatiana Akimova
January 6, 2026 AT 08:32Let's cut the noise-if you read the article you’ll see the key takeaways are solid, even if some details could be tighter.
Calandra Harris
January 17, 2026 AT 01:41Our nation's men deserve clear guidance not vague American studies.
Dan Burbank
January 27, 2026 AT 18:50One must ponder the epistemological abyss that this manuscript inhabits; it parades as a synthesis yet flirts with conjecture. The prose, while ornate, betrays a profound reluctance to engage with methodological rigor. In the grand theater of urological discourse, this contribution is a fleeting curtain call rather than a standing ovation.
Anna Marie
February 7, 2026 AT 11:58I appreciate your eloquent critique and would add that incorporating robust meta‑analytic techniques could elevate the discourse from theatrical flourish to substantive advancement.