Heart Arrhythmias from Medications: Warning Signs and What to Do
 Jan, 18 2026
Jan, 18 2026
Most people don’t think their daily pills could mess with their heart rhythm. But it happens more often than you’d guess. Over 400 common medications - from antibiotics to antidepressants - can trigger dangerous heart rhythm changes. These aren’t rare side effects. They’re real, measurable risks that send tens of thousands to the hospital every year. And the scary part? Many of these cases are preventable.
What Exactly Is a Drug-Induced Arrhythmia?
A drug-induced arrhythmia is when a medication causes your heart to beat too fast, too slow, or irregularly. It’s not just a flutter you feel once in a while. These are rhythm disturbances that can lead to fainting, stroke, or even sudden cardiac arrest. The most common type is QT prolongation, where the heart’s electrical cycle gets stretched out, making it vulnerable to a life-threatening rhythm called torsades de pointes.
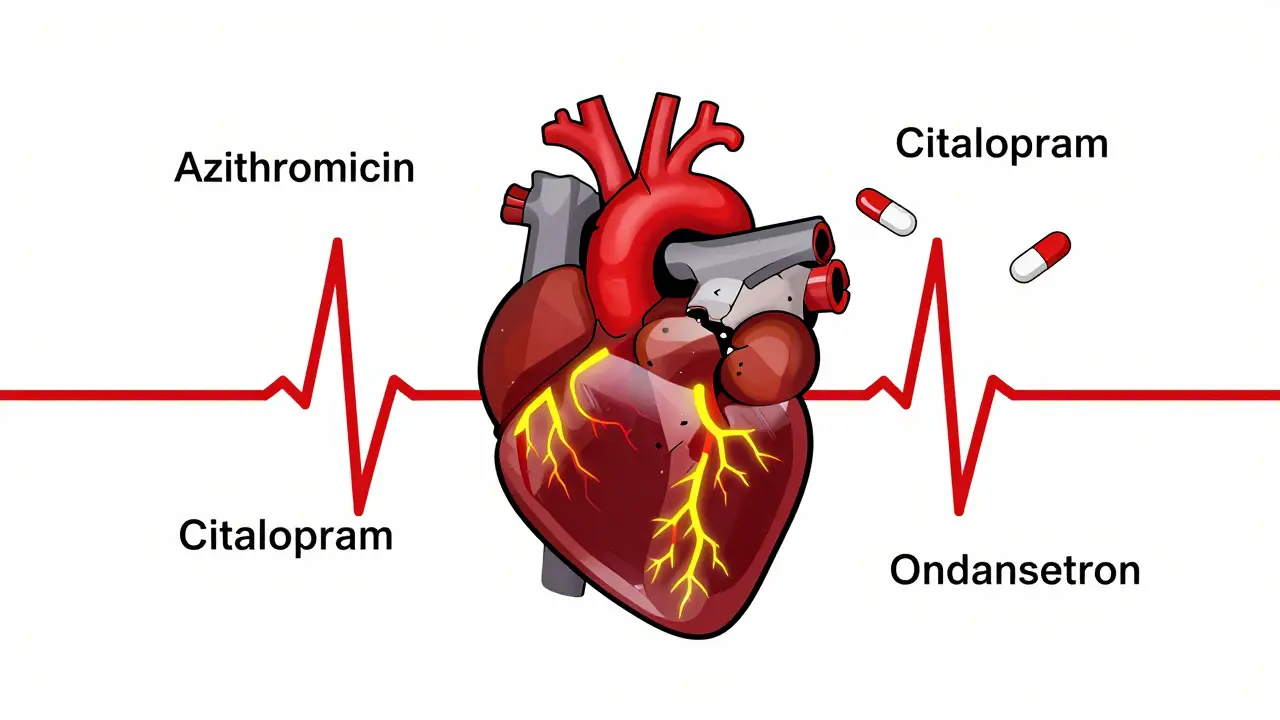
This isn’t limited to old-school drugs. Even antibiotics like azithromycin, antidepressants like citalopram, and cancer drugs like trastuzumab can do it. And here’s the twist: some of the drugs meant to fix arrhythmias - like flecainide or amiodarone - can actually cause them. That’s called proarrhythmia. It’s like trying to put out a fire with gasoline.
Who’s Most at Risk?
It’s not random. Certain people are far more likely to develop these problems. Age is a big one. About 60-70% of severe cases happen in people over 65. Why? Kidneys slow down with age, so drugs build up. Electrolytes drop. And older adults often take five or more medications at once.
Electrolyte imbalances are another major trigger. Low potassium (hypokalemia) and low magnesium (hypomagnesemia) are found in 20% and 10-15% of hospitalized patients with drug-induced arrhythmias, respectively. Even a small dip can turn a safe dose into a dangerous one.
Alcohol is a silent player. Drinking more than three drinks a day triples your risk. And if you smoke? That adds another layer of strain on your heart’s electrical system.
Genetics matter too. Around 15% of people of African ancestry carry the S1103Y variant, and 12% of East Asians carry R1193Q. These gene changes make heart cells extra sensitive to QT-prolonging drugs. Right now, routine genetic testing isn’t standard - but it’s coming fast. Some hospitals are already using it for high-risk patients before prescribing drugs like methadone or certain antipsychotics.
Common Medications That Can Trigger Arrhythmias
Here’s a real-world breakdown of the top offenders:
- Antibiotics - Macrolides (azithromycin, erythromycin) and fluoroquinolones (levofloxacin) prolong QT in 3-5% of users, especially in the first week. This is why doctors now avoid azithromycin if you’re on other QT-prolonging meds.
- Antidepressants - SSRIs like citalopram and escitalopram, and tricyclics like amitriptyline, can cause both QT prolongation and bradycardia. Doses above 20 mg/day of citalopram are now flagged as high risk.
- Antipsychotics - Haloperidol, ziprasidone, and thioridazine carry black box warnings from the FDA. They’re linked to sudden death in vulnerable patients.
- Antiarrhythmics - Ironically, drugs like flecainide and propafenone can turn atrial flutter into a dangerous wide-complex tachycardia. Amiodarone, while effective, causes atrial fibrillation in 2-5% of users due to thyroid disruption.
- Digoxin - Used for heart failure and atrial fibrillation, but toxic at levels above 2 ng/mL. Elderly patients with kidney issues are especially at risk. Symptoms include nausea, confusion, and irregular heartbeat.
- Beta-blockers - Metoprolol and atenolol are great for controlling heart rate, but if the dose is too high, they can cause dangerous bradycardia. Fatigue, dizziness, and fainting are common signs.
- Antiemetics - Ondansetron (Zofran) and promethazine are commonly used for nausea, but both carry QT prolongation risks, especially in IV form.
And don’t forget combinations. Taking two QT-prolonging drugs together? Risk jumps 300-500%. That’s why pharmacists now run automated checks when prescriptions are filled - and why you should always tell every doctor what you’re taking.
Warning Signs You Can’t Ignore
You don’t need an ECG to know something’s wrong. These symptoms are your body’s alarm system:
- Palpitations - Feeling your heart race, skip, or pound. Reported in 70-80% of cases.
- Dizziness or lightheadedness - Especially when standing up. This isn’t just aging - it could be your heart not pumping enough blood.
- Fatigue - Not just being tired. This is the kind where even walking to the mailbox leaves you drained.
- Chest discomfort - Not always sharp pain. Sometimes it’s pressure, tightness, or just a weird feeling.
- Fainting or near-fainting - This is the reddest of red flags. If you’ve passed out after starting a new med, get checked immediately.
And yes - caffeine can trigger palpitations in 25-30% of people. But don’t panic. Caffeine alone rarely causes serious arrhythmias. It’s the combo with meds that’s dangerous.
What to Do If You Suspect a Problem
If you notice any of those symptoms after starting a new drug, don’t wait. Don’t assume it’s ‘just side effects.’ Call your doctor or go to urgent care. Bring your medication list - all of it, including supplements and OTC pills.
Your doctor should check:
- A baseline ECG before starting high-risk meds
- A repeat ECG within 72 hours of starting
- Blood tests for potassium and magnesium - targets are potassium >4.0 mEq/L and magnesium >2.0 mg/dL
If the arrhythmia is mild and caught early, stopping or lowering the dose fixes it in 75-85% of cases. For beta-blocker-induced bradycardia, reducing the dose helps 60-70% of patients. But if your heart rate drops below 40 bpm and you’re dizzy or fainting, you might need a pacemaker - even if you still need the drug for your heart condition.
In rare cases (5-10%), catheter ablation is used to destroy the abnormal electrical pathway. Surgery? Less than 2% of cases. But prevention is always better than repair.
How to Stay Safe
Here’s what you can do right now:
- Keep a current list of every medication, supplement, and herb you take. Update it every time your doctor changes something.
- Ask your pharmacist: ‘Does this drug affect my heart rhythm?’ They’re trained to catch interactions.
- Don’t skip electrolyte checks. If you’re on diuretics, make sure your potassium and magnesium are monitored regularly.
- Limit alcohol. More than three drinks a day is a known risk multiplier.
- Get moving. Daily 30-minute walks improve heart rhythm stability and help your body process meds better.
- Sleep 7-9 hours. Poor sleep raises stress hormones that destabilize heart rhythms.
And if you’re over 65, on multiple meds, or have kidney disease - be extra cautious. Your body doesn’t clear drugs like it used to. What was safe at 50 might be risky at 70.
The Future: Personalized Medicine Is Here
Doctors are starting to use genetic tests before prescribing. If you carry the S1103Y or R1193Q variant, they’ll avoid certain drugs altogether. New tools, like the ACC’s clinical decision support system launching in 2024, will scan your age, meds, electrolytes, and genetics to give you a personalized risk score.
Right now, the FDA has added black box warnings to 25 drugs since 2010 - eight of them in 2022 alone. That’s not bureaucracy. That’s real people dying from preventable causes.
Experts predict a 30-40% drop in severe cases over the next five years - if we act now. Better awareness. Better testing. Better communication between patients and providers.
You don’t have to live in fear of your meds. But you do need to be informed. Your heart is counting on it.
Can over-the-counter meds cause heart arrhythmias?
Yes. Common OTC drugs like pseudoephedrine (in cold medicines), certain antihistamines like diphenhydramine (Benadryl), and even high-dose herbal supplements like licorice root can trigger arrhythmias. Pseudoephedrine can raise heart rate and blood pressure, while diphenhydramine has QT-prolonging effects similar to prescription antihistamines. Always check labels and talk to your pharmacist before using OTC meds if you’re on heart meds or have a history of rhythm problems.
Is it safe to keep taking a medication if I feel palpitations?
No. Palpitations after starting a new drug are a red flag, not a nuisance. Don’t wait to see if they go away. Stop the medication only if your doctor advises it, but do not ignore the symptom. Call your doctor immediately. They may order an ECG or blood tests to check for electrolyte imbalances or drug toxicity. Many arrhythmias are reversible if caught early.
Can stress or anxiety mimic drug-induced arrhythmias?
Yes, anxiety can cause palpitations, rapid heartbeat, and dizziness - symptoms that overlap with drug-induced arrhythmias. But here’s the difference: anxiety-related palpitations usually happen during emotional stress and fade when you calm down. Drug-induced ones happen regardless of mood, often after taking the pill, and may be accompanied by fainting, chest pressure, or prolonged fatigue. If you’re unsure, get an ECG. It’s the only way to know for sure.
How long does it take for a drug-induced arrhythmia to go away after stopping the medication?
It varies. For QT prolongation, the ECG usually returns to normal within 3-7 days after stopping the drug. But if electrolytes are low, it can take longer - sometimes up to two weeks - until potassium and magnesium are restored. In cases of digoxin toxicity or amiodarone-induced issues, the drug can linger in your system for weeks or months, so symptoms may persist. Always follow up with your doctor for repeat testing.
Are there any supplements that help prevent medication-related arrhythmias?
Magnesium and potassium supplements can help if you’re deficient - but only under medical supervision. Taking them without testing can be dangerous. Too much potassium can cause cardiac arrest. Too much magnesium can lower blood pressure too much or cause muscle weakness. The best way to prevent arrhythmias is through diet: bananas, spinach, avocados, nuts, and beans for potassium; almonds, dark chocolate, and leafy greens for magnesium. Don’t self-prescribe supplements - get tested first.
Should I get genetic testing for arrhythmia risk before starting a new drug?
It’s not routine yet - but it should be if you’re prescribed a high-risk drug like methadone, certain antidepressants, or antipsychotics, especially if you’re over 65, have a family history of sudden cardiac death, or have had unexplained fainting. Some hospitals in Australia and the U.S. now offer pre-prescription genetic screening for these cases. Ask your cardiologist or pharmacist if it’s available. The cost is dropping, and the benefit is life-saving.
What Comes Next?
If you’re on a medication that could affect your heart rhythm, don’t stop it cold turkey. Talk to your doctor. Get an ECG. Check your electrolytes. Review every pill you take - even the ones you think are harmless.
The goal isn’t to scare you off meds. It’s to make sure you’re using them safely. Millions of people take these drugs without issue. But for those who are vulnerable, a simple check could mean the difference between a quiet morning and a trip to the ER.
Know your meds. Know your body. And never ignore a heartbeat that feels off.

Erwin Kodiat
January 19, 2026 AT 23:33Wow, this is one of those posts that makes you pause and actually think about what’s in your medicine cabinet. I never realized something as simple as Zofran could mess with your heart rhythm. Thanks for laying it out so clearly - this isn’t fearmongering, it’s practical wisdom.
Valerie DeLoach
January 20, 2026 AT 14:16I’m a nurse in a geriatric unit, and I see this every day. An elderly patient on five meds, no electrolyte monitoring, and then they faint at the grocery store. It’s not ‘just old age’ - it’s polypharmacy + ignorance. This post should be mandatory reading for anyone over 60, or caring for someone who is.
Aman Kumar
January 21, 2026 AT 20:30Let me be blunt: Big Pharma doesn’t want you to know this. They profit from your arrhythmias. The FDA’s black box warnings? Too little, too late. They’ve known about QT prolongation for decades - but they buried the data until lawsuits piled up. Genetic testing isn’t ‘coming’ - it’s been suppressed because it’s too expensive to screen everyone. Wake up.
sujit paul
January 23, 2026 AT 02:44One must contemplate the metaphysical implications of pharmacological agency. The body, a temple of electrochemical symphony, is now subject to the arbitrary whims of molecular interference. Are we not, in essence, becoming pharmacological puppets? The pharmaceutical-industrial complex has weaponized our trust - and the heart, that most sacred rhythm, has become a statistical variable in a profit algorithm.
Josh Kenna
January 24, 2026 AT 06:36ok so i just started citalopram last week and i’ve been feeling like crap - dizzy, tired, heart feels weird - and i thought it was just anxiety or me being a wuss. this post just scared the shit out of me. i’m calling my doc tomorrow. also i took benadryl last weekend for allergies. did i just almost die??
Jake Rudin
January 25, 2026 AT 16:42...And yet... we continue... to swallow... the pills... without question... because... convenience... trumps... caution... and... corporate... logos... are... more... trusted... than... our... own... bodies...
Astha Jain
January 26, 2026 AT 21:02OMG i had no idea licorice root could do this?? i’ve been eating it like candy bc it’s ‘natural’ and ‘good for stress’ - wait… so i’m basically doing drugs?? 😱
Phil Hillson
January 28, 2026 AT 07:17This is just another fear post from someone who wants clicks. Everyone gets palpitations sometimes. You’re telling people to panic over every little flutter. I’ve been on amiodarone for 8 years and I’m fine. Stop scaring people.
Christi Steinbeck
January 29, 2026 AT 01:15YOU ARE NOT ALONE. I felt the same way after starting Zofran - like my heart was trying to escape my chest. I called my pharmacist, they flagged it, we switched meds, and I’m fine now. Don’t wait. Don’t ignore. Don’t feel silly. Your heart isn’t being dramatic - it’s screaming. Listen.