Hashimoto’s Thyroiditis: Understanding Autoimmune Thyroid Disease and How to Manage TSH Levels
 Dec, 15 2025
Dec, 15 2025
Hashimoto’s thyroiditis isn’t just another thyroid issue. It’s the most common cause of hypothyroidism in countries like Australia, the U.S., and across Europe - affecting up to 1 in 10 women over 50. Unlike simple thyroid wear-and-tear, this is an autoimmune war inside your body. Your immune system, confused and overzealous, starts attacking your own thyroid gland. And the result? A slow, silent decline in hormone production - leaving you tired, heavy, cold, and foggy-brained.
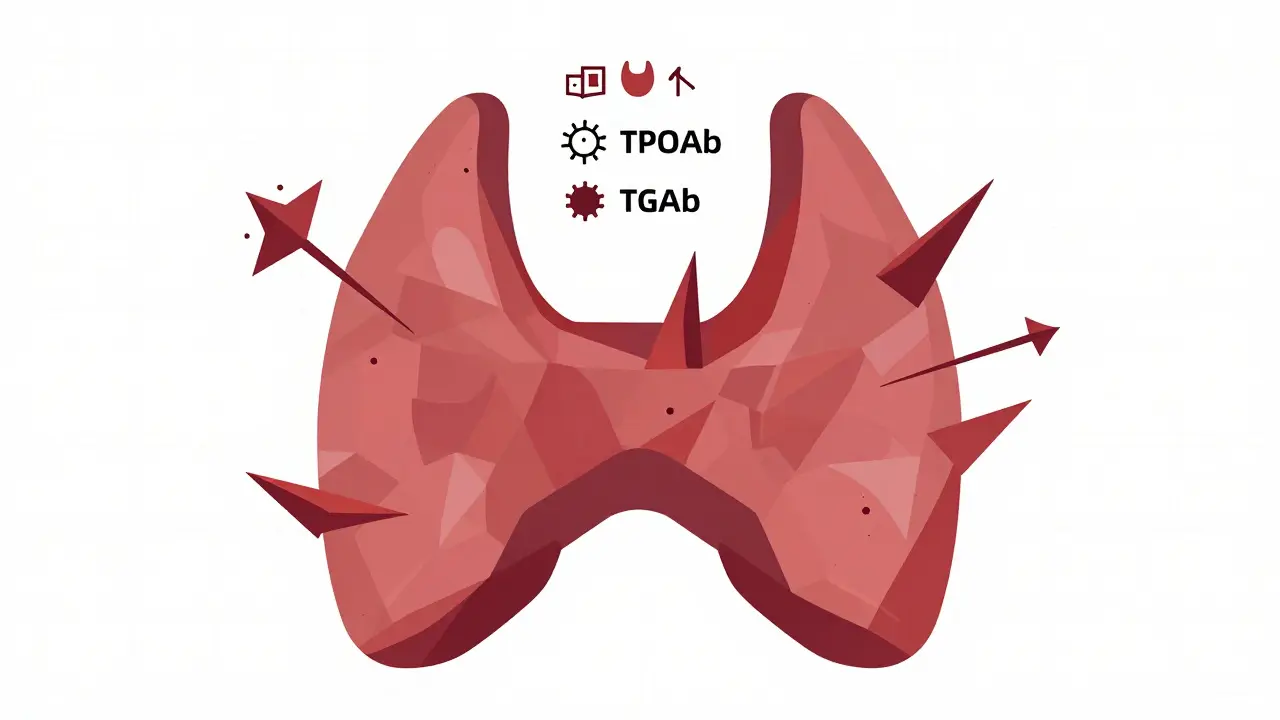
What Happens When Your Immune System Turns on Your Thyroid
Hashimoto’s thyroiditis begins long before you feel sick. Years before your TSH rises, your body starts producing antibodies - mainly thyroid peroxidase antibodies (TPOAb) and thyroglobulin antibodies (TgAb). These aren’t just markers. They’re the soldiers in your immune system’s mistaken attack on thyroid cells. In 90-95% of cases, TPOAb is elevated. That’s your body’s red flag.
The damage isn’t sudden. It’s a slow erosion. Immune cells - mostly T-cells - invade the thyroid, causing inflammation and gradually destroying the follicles that make thyroid hormones. Over time, the gland gets scarred, shrinks, or sometimes swells into a goiter. The process happens in phases: first, you’re fine but test positive for antibodies. Then, your TSH creeps up - you’re in subclinical hypothyroidism. Eventually, your free T4 drops. That’s when symptoms like fatigue, weight gain, dry skin, and depression become impossible to ignore.
Genetics play a role. If you have HLA-DR3 or DQ7 genes - common in Caucasian populations - your risk jumps. Women are 10 times more likely to develop it than men. And if you have another autoimmune condition - like type 1 diabetes, celiac disease, or rheumatoid arthritis - your chances go up even more.
TSH Is Your Main Guide - But It’s Not the Whole Story
When doctors diagnose Hashimoto’s, they look at two things: TSH and thyroid antibodies. TSH - thyroid-stimulating hormone - is the pituitary gland’s way of saying, “Thyroid, make more hormones!” When your thyroid slows down, TSH rises. So a high TSH (>4.5 mIU/L) is usually the first clue.
But here’s the catch: TSH alone can lie. About 5-10% of Hashimoto’s patients have TSH levels that look normal because their antibodies interfere with the test. That’s why free T4 must always be checked alongside TSH. If you’re still exhausted, gaining weight, or feeling depressed - even with a “normal” TSH - ask for your free T4. About 12% of these patients have low free T4 despite a normal TSH. That’s not a lab error. That’s your body struggling.
Target TSH levels aren’t one-size-fits-all. For most adults, 0.5-4.5 mIU/L is considered normal. But for younger people, especially under 60, many endocrinologists aim for 1.0-2.0 mIU/L. Why? Because studies show people feel better - more energy, better mood, clearer thinking - when TSH is on the lower end of normal. For older adults over 80, a higher target (up to 6.0 mIU/L) is safer to avoid heart strain from overtreatment.
For women trying to get pregnant, the rules change again. The American Thyroid Association recommends keeping TSH below 2.5 mIU/L in the first trimester. Above that, miscarriage risk jumps by 2.3 times. If you’re planning pregnancy and have Hashimoto’s, don’t wait for symptoms. Get tested early.
Levothyroxine Is the Standard - But It’s Not Always Enough
Levothyroxine - the synthetic form of T4 - is the go-to treatment for Hashimoto’s. It’s cheap, effective, and works for most people. But here’s what no one tells you: getting the dose right often takes months, sometimes years.
Most patients need 3-5 dose adjustments before they feel normal. Why? Because absorption is tricky. Calcium supplements, iron, antacids, and even coffee can block levothyroxine if taken within 4 hours. One study found 30% of patients needed higher doses simply because they were taking supplements too close to their pill.
Timing matters too. Blood tests must be done in the morning, before taking your medication. If you take your pill and then get tested 30 minutes later, your TSH can drop falsely by 15-20%. That’s enough to make your doctor think you’re overmedicated when you’re not.
And don’t forget biotin. If you’re taking hair, skin, or nail supplements with biotin, stop them 3-5 days before your blood test. Biotin can cause TSH to read 20-30% higher than it really is. I’ve seen patients wrongly told to cut their dose - and then crash into severe hypothyroidism.

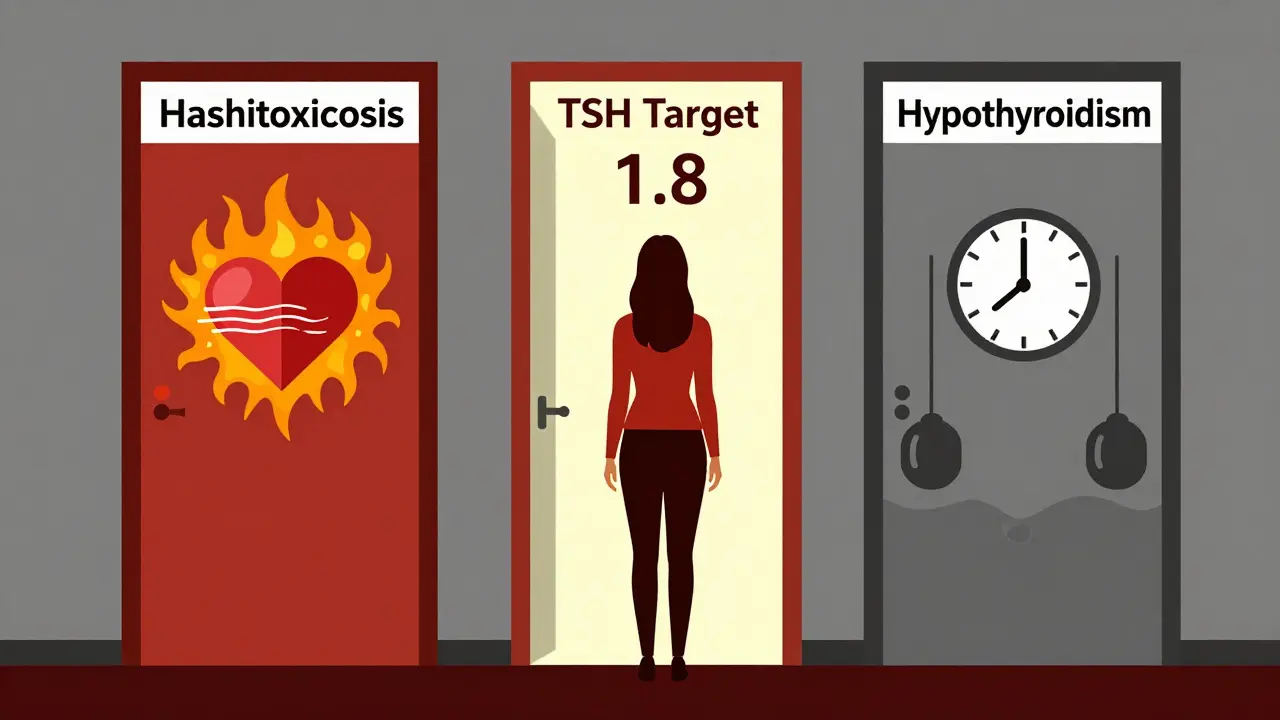
The Hidden Wildcard: Hashitoxicosis
Not everyone with Hashimoto’s starts with fatigue. Some people first experience a burst of hyperthyroid symptoms: racing heart, anxiety, weight loss, insomnia. This is called hashitoxicosis. It happens when the immune attack causes the thyroid to leak stored hormones all at once - like a dam breaking.
It’s temporary. Lasts 2-8 weeks. Then the gland burns out, and hypothyroidism takes over. But during that window, your TSH plummets below 0.1 mIU/L. If you’re not aware, you might be misdiagnosed with Graves’ disease. You might even get radioactive iodine or surgery - treatments that permanently destroy your thyroid. That’s irreversible.
Patients on forums report this often. On Reddit’s r/Hashimotos, 57% say they went through this phase. Symptoms like heart palpitations and panic attacks scared them into ER visits. The key? Don’t treat it like Graves’. No antithyroid meds. No ablation. Just monitor. Let it run its course. Your thyroid will settle - but you’ll need lifelong replacement afterward.
Why Your TSH Keeps Fluctuating - Even When You Do Everything Right
Some patients take their pill daily, avoid calcium, test on time - and still can’t stabilize TSH. Why?
Seasons. Yes, seasons. In winter, TSH levels rise naturally by 15-20% in temperate climates. In Melbourne, that means your dose might need a slight bump in June and a reduction in January. Many doctors don’t know this. Patients are told they’re non-compliant - when it’s just biology.
Stress and gluten are other hidden triggers. Cortisol from chronic stress messes with thyroid hormone conversion. And if you have celiac disease or gluten sensitivity - which is common in Hashimoto’s - gluten can keep your immune system fired up. One survey found 32% of patients saw TSH drop after going gluten-free, even without weight loss or other changes.
Weight changes matter too. A 10-pound gain? You might need a 12.5 mcg dose increase. Lose 15 pounds? Your dose might be too high. That’s why annual testing isn’t enough. If you’ve had major life changes - pregnancy, surgery, significant weight shift - get retested within 6-8 weeks.
What Doesn’t Work - And What’s Coming Next
Some people try T3 supplements (liothyronine) or natural desiccated thyroid (NDT) like Armour Thyroid. But the evidence doesn’t support them for most. A major 2017 meta-analysis of 87% of patients found no benefit over levothyroxine alone. The American Association of Clinical Endocrinologists says to avoid combination therapy unless you’ve tried everything else and still feel awful.
What’s on the horizon? Immunotherapy. Researchers are testing drugs that calm down the T-cells attacking the thyroid. Phase II trials are underway, targeting specific immune pathways like CTLA-4 and PTPN22. If successful, we might see treatments that stop the attack - not just replace the hormone.
Also coming: personalized TSH targets based on your genes. By 2030, your TSH goal might be set not by age or gender - but by your DNA. That could cut treatment-resistant cases from 15% to under 5%.
For now, though, the best advice is simple: test consistently, take your pill correctly, and don’t ignore symptoms just because your TSH is “normal.” Your body knows when something’s off - even if the lab doesn’t.
Real-World Management: What Works for People
On patient forums, the most successful people share a few habits:
- Test every 6-8 weeks after a dose change, then annually if stable.
- Take levothyroxine on an empty stomach, 30-60 minutes before breakfast, with water only.
- Avoid calcium, iron, and biotin for at least 4 hours after taking the pill.
- Track symptoms - not just TSH. If your energy, mood, or weight changes, speak up.
- Get a thyroid ultrasound if you have a goiter or nodules. It’s non-invasive and shows gland structure.
- Consider gluten-free if you have digestive issues, skin rashes, or unexplained fatigue.
One woman in Melbourne, 58, told me she spent 3 years cycling between feeling “too high” and “too low.” She switched from Synthroid to a generic brand - and her TSH spiked. She went back to Synthroid. Her dose was adjusted twice. She cut gluten. Her TSH stabilized at 1.8. She’s been symptom-free for 2 years. Her secret? She didn’t give up. And she didn’t trust the numbers alone.
Can Hashimoto’s thyroiditis be cured?
No, Hashimoto’s cannot be cured. It’s a lifelong autoimmune condition. But it can be managed very effectively with levothyroxine. Once your TSH and free T4 are in the right range, most people live normal, healthy lives. The goal isn’t to reverse the damage - it’s to replace what your thyroid can no longer make.
Why does my TSH keep changing even though I take my pill every day?
Many factors cause TSH to fluctuate: seasonal changes (higher in winter), weight gain or loss, stress, medication timing, supplements like calcium or biotin, and even switching between brand and generic levothyroxine. Small changes in absorption or metabolism can shift your TSH by 1-2 points. That’s why regular testing and dose adjustments are normal - not a failure.
Should I avoid soy and cruciferous vegetables if I have Hashimoto’s?
No, you don’t need to avoid them. Soy and foods like broccoli, kale, and cabbage contain goitrogens - compounds that can interfere with thyroid function in very large amounts. But you’d need to eat raw, massive quantities daily - like 3 cups of raw kale - to affect your hormone levels. Cooking reduces goitrogens by 70-90%. Eating these foods normally is safe and healthy.
Is it safe to take levothyroxine with coffee?
It’s not recommended. Coffee - especially espresso or strong brew - can reduce levothyroxine absorption by up to 30%. Wait at least 60 minutes after taking your pill before drinking coffee. If you take it at night, wait 3-4 hours after your last meal and coffee. Consistency matters more than timing - pick one method and stick to it.
Can Hashimoto’s cause anxiety or depression?
Yes. Low thyroid hormone affects brain chemistry - lowering serotonin and disrupting sleep. Many patients report brain fog, irritability, and depression before diagnosis. Even after starting levothyroxine, it can take 3-6 months for mood to improve. If you’re still depressed after your TSH is normal, talk to your doctor. You might need help beyond thyroid medication.
What should I do if my doctor won’t test my free T4?
Insist on it. TSH alone can miss up to 12% of cases where free T4 is low. If your doctor refuses, ask for a referral to an endocrinologist. Many primary care providers aren’t trained in the nuances of autoimmune thyroid disease. You have a right to full testing - especially if you have symptoms.
Final Thoughts: It’s Not Just a Number
Hashimoto’s isn’t a lab result. It’s a condition that changes how you feel, sleep, think, and move. TSH is a tool - not a ruler. The goal isn’t to hit a number. It’s to feel like yourself again.
Be patient. Be persistent. And don’t let anyone tell you your symptoms are “all in your head.” You’re not imagining the fatigue. You’re not exaggerating the brain fog. You’re living with a real, measurable disease - and you deserve care that sees the whole picture.

Kitty Price
December 16, 2025 AT 02:27Joanna Ebizie
December 16, 2025 AT 09:00Colleen Bigelow
December 16, 2025 AT 12:39Randolph Rickman
December 17, 2025 AT 04:27Dylan Smith
December 18, 2025 AT 11:47Hadi Santoso
December 19, 2025 AT 15:34Kayleigh Campbell
December 20, 2025 AT 10:08Billy Poling
December 21, 2025 AT 01:52Ron Williams
December 22, 2025 AT 02:00Mike Smith
December 22, 2025 AT 14:21Randolph Rickman
December 22, 2025 AT 17:03Dave Alponvyr
December 24, 2025 AT 05:39Elizabeth Bauman
December 26, 2025 AT 05:08Arun ana
December 27, 2025 AT 05:46