Calcium Supplements vs Bisphosphonates: How to Prevent Absorption Issues
 Oct, 24 2025
Oct, 24 2025
Bisphosphonate Calcium Timing Calculator
Find the safe timing window to maximize the effectiveness of your bisphosphonate medication while safely taking calcium supplements. Based on FDA guidelines and clinical studies, this tool helps you avoid the 90% absorption loss that occurs when calcium and bisphosphonates are taken too close together.
How This Works
Key rule: Take calcium supplements at least 2 hours after taking your bisphosphonate.
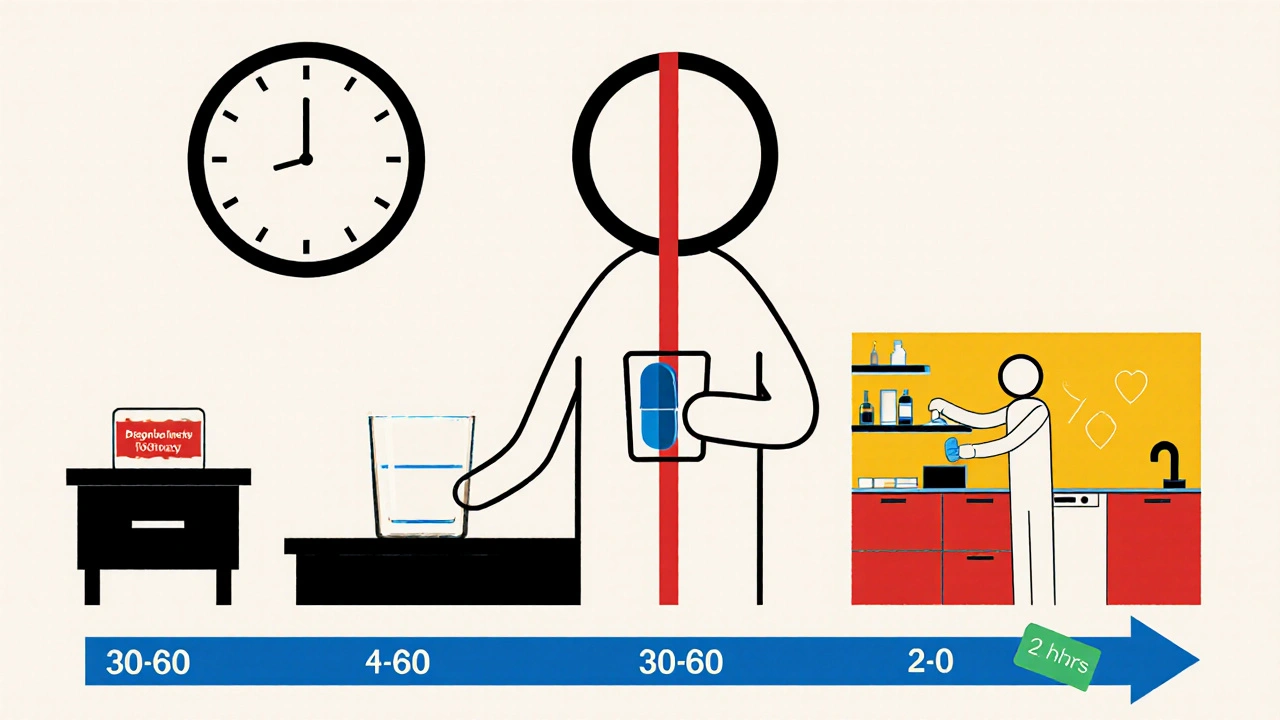
Your bisphosphonate needs to be taken on an empty stomach with water. After taking it, you must wait 30-60 minutes before eating or taking other medications (see table below).
Your Timing Recommendations
Minimum waiting period after bisphosphonate: 30 minutes
Earliest time to take calcium: 07:30
Total gap required: 2 hours
Why this matters: Up to 94% absorption loss
Important Notes
Always take bisphosphonates with a full glass of plain water on an empty stomach. Stay upright for at least 30-60 minutes after taking the dose. If you miss the timing window, don't panic - just continue your regular schedule.
When you’re on a bone‑strengthening plan, the last thing you want is a hidden clash that wipes out half of what you’re paying for. Calcium supplements and bisphosphonates are the classic example - take them together and you can lose up to 90% of the drug’s effect. This guide walks you through why the interaction happens, which drugs are most sensitive, and practical steps to keep your regimen on track.
What are bisphosphonates and how do they work?
Bisphosphonates are synthetic compounds that attach to bone surfaces and block the cells that break down bone (osteoclasts). By slowing resorption, they cut fracture risk by 40‑70% in people with osteoporosis, according to the Fracture Intervention Trial.
First‑generation agents like etidronate appeared in the 1960s, but today most patients use nitrogen‑containing versions such as alendronate, risedronate, ibandronate (oral) or zoledronic acid (intravenous). Oral forms are cheap and convenient, but they have a notorious downside: less than 1% of an oral dose actually enters the bloodstream.
Why calcium interferes with bisphosphonate absorption
Both calcium ions and bisphosphonates love to bind to phosphate groups. In the gut, calcium forms an insoluble complex with the drug, turning it into a crystal that can’t cross the intestinal wall. A 2019 study in the Journal of Clinical Pharmacology showed a 94% drop in alendronate absorption when taken with calcium carbonate.
Other calcium salts behave similarly. Calcium citrate cuts alendronate uptake by about 88%, while calcium gluconate still knocks down absorption by roughly 70%.
The chemistry is simple, but the impact on patients is huge - missed absorption means lower bone density gains, higher fracture risk, and wasted money.
Timing rules that actually work
The FDA‑approved label for every oral bisphosphonate spells out the same core steps:
- Take the tablet with a full glass of plain water (no coffee, juice, or milk).
- Do this after an overnight fast of at least 8 hours.
- Remain upright (sitting or standing) for the next 30 minutes (alendronate) or 60 minutes (risedronate, ibandronate).
- Only after the waiting period can you eat, drink, or take other meds.
- Schedule calcium supplements for at least 2 hours after the bisphosphonate dose.
These steps cut the chance of the drug binding to calcium and also protect the esophagus from irritation - 62% of GI side effects happen when patients lie down within the first hour.
Comparing oral bisphosphonates and their calcium sensitivity
| Drug | Typical dose | Fasting window | Calcium carbonate impact | Notes |
|---|---|---|---|---|
| Alendronate (Fosamax) | 70 mg weekly | 30 min | ‑94% | Strict timing critical |
| Risedronate (Actonel) | 35 mg weekly or 150 mg monthly | 60 min | ‑88% | Slightly more food‑tolerant |
| Ibandronate (Boniva) | 150 mg monthly | 60 min | ‑90% (est.) | Monthly dose offers a bit of flexibility |
Even the “most tolerant” drug still loses close to 90% of its effect if you sip a calcium‑rich beverage right after the tablet.
Intravenous options: when timing isn’t an issue
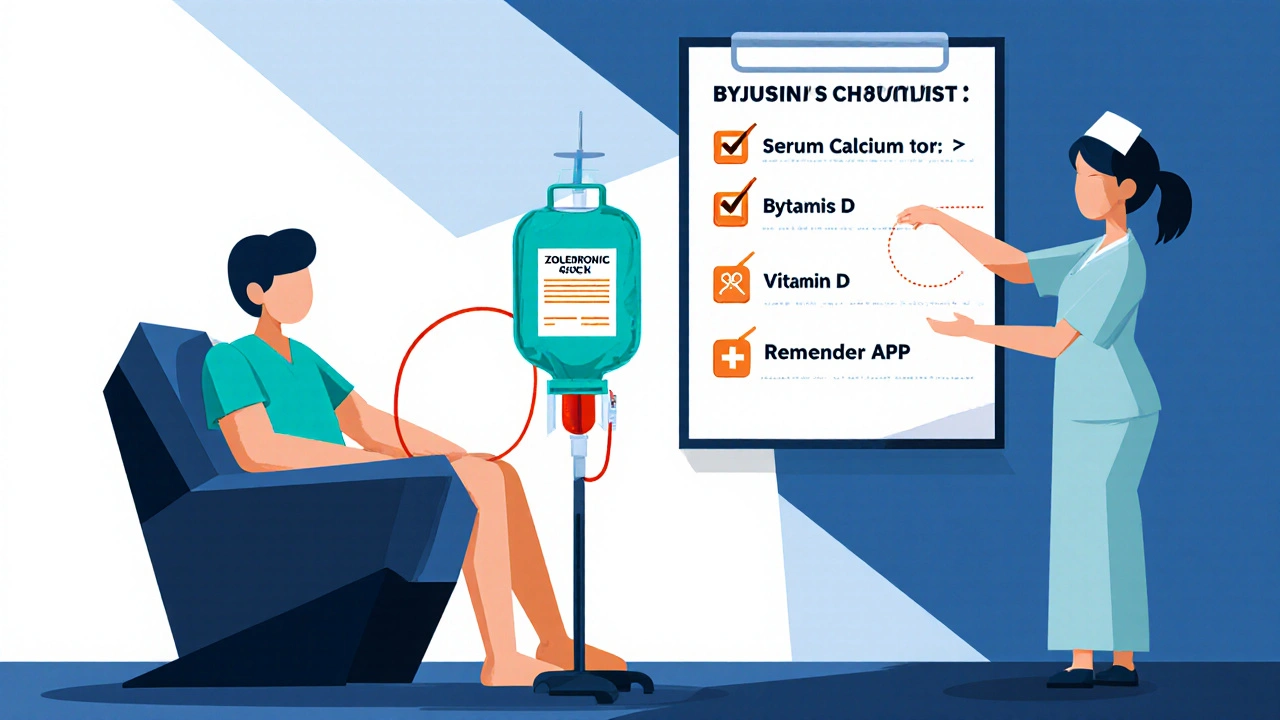
Zoledronic acid (Reclast) is given as a 5 mg IV infusion once a year. Because the drug bypasses the gut, calcium in the diet does not interfere with its absorption. The downside is a 15‑30% chance of an acute‑phase reaction - flu‑like symptoms, fever, and a brief dip in serum calcium. Monitoring calcium levels before the infusion is mandatory, especially in patients with kidney disease.
Practical tips for everyday life
Putting the timing rules into a daily routine can feel like a choreography, but a few tricks make it easier:
- Morning ritual: Keep your bisphosphonate and a full glass of water on the nightstand. Set a phone alarm for the exact wait time, then move straight to the kitchen for coffee.
- Pill organizers: Label compartments “Bisphosphate AM” and “Calcium PM” - one patient reported a 6.2% rise in hip bone density after 18 months of using this system.
- Combine vitamin D with dinner: Vitamin D improves calcium uptake, so take it with your evening meal rather than the morning dose.
- Use reminder apps: The National Osteoporosis Foundation’s free app sends push notifications with exact timing cues; users see a 65% jump in adherence.
- Schedule other meds: Take blood pressure or thyroid pills only after the bisphosphonate waiting period, as advised by Mayo Clinic.
For patients with GERD or esophageal strictures, lying down is painful. In those cases, a switch to IV zoledronic acid or to a newer agent like denosumab (which has no oral timing constraints) may be the better path.
When things go wrong: troubleshooting common pitfalls
Problem: You accidentally take calcium within an hour of the bisphosphonate.
Solution: Don’t panic. Keep a log of the mistake, inform your prescriber, and continue the regimen as usual. One missed dose rarely causes a fracture, but repeated errors lower efficacy.
Problem: Persistent esophageal irritation despite upright posture.
Solution: Switch to a different oral bisphosphonate with a monthly dose (ibandronate) or discuss IV therapy with your doctor.
Problem: Low serum calcium before an IV infusion.
Solution: Supplement with calcium-rich foods (dairy, leafy greens) and possibly a short‑term oral calcium under supervision, then re‑check labs before the infusion.
What the experts say
Dr. Ethel Siris, former N.O.F. president, calls timing “the single most common reason for bisphosphonate failure.” Osteoporosis Canada’s 2023 guidelines echo this, recommending a minimum 2‑hour gap between the drug and any calcium source.
Conversely, Dr. Andrea Singer warns that “inconsistent but continued use is preferable to stopping altogether.” If the timing rules feel impossible, discuss alternative therapies rather than abandoning treatment.
Future directions: less timing‑sensitive drugs
Researchers are testing enteric‑coated alendronate that can be taken with food and still achieve 38% higher absorption. Early phase‑2 data are promising, but the drug won’t be on shelves until at least 2027.
Meanwhile, newer agents like denosumab (a monoclonal antibody) or abaloparatide (a PTH‑related peptide) bypass the gut entirely, but they come at a steep price-often $2,000‑$3,000 per month compared with $15‑$50 for generic bisphosphonates.
Bottom line checklist
- Confirm baseline serum calcium > 8.5 mg/dL and 25‑hydroxyvitamin D > 30 ng/mL before starting.
- Take oral bisphosphonate with plain water after an overnight fast.
- Wait 30‑60 minutes, stay upright, then eat or take other meds.
- Schedule calcium supplements at least 2 hours later, preferably with dinner.
- Consider IV zoledronic acid if oral timing is too tough.
- Use a phone alarm, pill organizer, or reminder app to stay on track.
- Re‑check serum calcium and vitamin D every 6 months.
Can I take calcium and bisphosphonates at the same time if I drink a lot of water?
No. Even with plenty of water, calcium binds to the drug in the gut and creates an insoluble complex. The water doesn’t prevent that chemical reaction, so the absorption loss remains around 90%.
Is coffee considered a food that interferes with bisphosphonate absorption?
Yes. Coffee (and tea, juice, milk) contains calcium or other minerals that can cut absorption by 50‑60%. It’s safest to wait the full fasting period before your first sip.
What should I do if I miss the 2‑hour window after taking my bisphosphonate?
Take your calcium supplement later in the day and continue the next dose as scheduled. One missed timing isn’t catastrophic, but try to avoid repeats.
Are intravenous bisphosphonates completely free of calcium interactions?
They bypass the gut, so calcium in food or supplements does not affect the drug’s efficacy. However, you still need adequate calcium stores before the infusion to prevent low blood calcium after the dose.
How often should I have my blood calcium checked while on bisphosphonates?
Guidelines recommend checking serum calcium and vitamin D every six months, especially if you have kidney disease or are on IV therapy.

Kester Strahan
October 24, 2025 AT 16:38Yo, the calcium‑bisphosphonate chemeistry is basically a binding showdown – calcium ions lock up the drug like a glove on a nail. If you pop your alendronate with a calcium pill, you’re slashing absorption by about 90%, which is a massive waste of cash and bone‑health potential. So, schedule ’em far apart and keep that gut chemistry in your favor.
Doreen Collins
October 31, 2025 AT 09:30Totally get how overwhelming the timing can feel; think of it like a daily choreography that just needs a few cues. Setting your alarm for the 30‑minute wait and using a pill organizer can turn chaos into a smooth routine.
HILDA GONZALEZ SARAVIA
November 7, 2025 AT 03:23For anyone on a weekly alendronate schedule, the critical window is absolutely non‑negotiable – you need an empty stomach, a full glass of water, and then stay upright for at least half an hour. The literature shows a 94% drop in absorption with calcium carbonate, so timing isn’t just a suggestion, it’s a requirement. If you’re prone to forgetting, there are smartphone apps that send push notifications exactly when you need to act. Also, consider pairing your calcium supplement with dinner, which naturally gives you that two‑hour buffer.
Dason Avery
November 13, 2025 AT 21:15Hey there! 🌟 Remember, the upright rule isn’t just about absorption – it also protects your esophagus from irritation. A quick stand‑up after your dose can save you from that burning feeling later. And don’t stress if you miss a day; just get back on track, the body’s not going to crumble over one slip. Keep the vibe positive and stay consistent! 🙌
Casey Morris
November 20, 2025 AT 15:08Indeed; the pharmacokinetic profile of bisphosphonates is profoundly altered by concurrent calcium intake; therefore, adherence to the fasting protocol is paramount; neglecting this step results in a precipitous decline in bioavailability, practically nullifying therapeutic benefit.
Teya Arisa
November 27, 2025 AT 09:00Dear community, I would like to emphasize that maintaining serum calcium levels above 8.5 mg/dL prior to initiating therapy is essential for safety and efficacy. Furthermore, scheduling calcium supplementation with the evening meal aligns with the recommended two‑hour separation, thereby optimizing bone mineral accrual. 😊
Marilyn Pientka
December 4, 2025 AT 02:52It is frankly irresponsible to disregard established guidelines when patient outcomes are at stake; the ethical imperative demands rigorous compliance with the absorption timing to prevent iatrogenic failure of treatment. Non‑adherence not only jeopardizes skeletal integrity but also constitutes a dereliction of fiduciary duty towards healthcare resources.
Jordan Levine
December 10, 2025 AT 20:45Listen up, folks! 🇺🇸 Our veterans and seniors deserve the best-no one should be messing up their bone meds with cheap calcium shortcuts. Follow the protocol or you’ll be putting your own health at risk, and that’s just unacceptable. 💪
Carla Taylor
December 17, 2025 AT 14:37Guys, just set a reminder on your phone for the 30‑minute wait and keep a glass of water nearby. Simple hack that saves you from a lot of hassle.
Lindy Hadebe
December 24, 2025 AT 08:30Data consistently shows a near‑90% reduction in bisphosphonate absorption when taken with calcium, reinforcing the need for strict timing adherence.
Mary Mundane
December 31, 2025 AT 02:22One missed window won’t break your treatment.
Michelle Capes
January 6, 2026 AT 20:14I always keep my bisphos in the nightstand and use a sticky note to remind me to wait - it’s super helpful! :)
Tammy Watkins
January 13, 2026 AT 14:07In the grand tapestry of osteoporosis management, the temporal choreography between bisphosphonate administration and calcium supplementation emerges as a linchpin of therapeutic success. First, the pharmacodynamic principle dictates that calcium ions, upon encountering the drug within the gastrointestinal milieu, forge a stable, insoluble complex impervious to intestinal translocation. Consequently, the anticipated osteoclast inhibition is dramatically attenuated, eroding the very foundation upon which fracture risk reduction is built. Second, clinical trials have unequivocally quantified this interaction, revealing absorption decrements approaching ninety percent-a figure that translates into a substantial loss of clinical benefit. Third, the practical implications for the patient are manifold: diminished bone mineral density gains, heightened susceptibility to fracture, and the financial burden of wasted medication. Fourth, the prescribed mitigation strategy-fasting, water-only ingestion, upright posture, and a two‑hour calcium gap-constitutes a rigorously validated protocol that restores absorption to near‑optimal levels. Fifth, adherence to this regimen is facilitated by modern tools such as smartphone alerts, pill organizers bearing distinct labels, and patient education initiatives championed by osteoporosis foundations. Sixth, for individuals with comorbidities such as gastroesophageal reflux disease, the upright requirement also serves to prevent mucosal irritation, underscoring a dual protective role. Seventh, alternative therapeutic avenues, including intravenous zoledronic acid or subcutaneous denosumab, bypass the gastrointestinal tract altogether, offering viable options for those unable to honor the timing constraints. Eighth, however, these alternatives carry their own risk profiles and cost considerations, necessitating a personalized risk‑benefit analysis. Ninth, the clinician’s role in reinforcing the timing doctrine cannot be overstated; clear communication and periodic review of patient technique are essential. Tenth, the broader public health perspective recognizes that widespread adherence to timing guidelines could substantially lower the epidemiological burden of osteoporotic fractures. Eleventh, ongoing research into enteric‑coated formulations promises to alleviate the timing dilemma in future generations of therapy. Twelfth, until such innovations become mainstream, the onus remains on patients and providers alike to respect the chemistry that governs drug efficacy. Thirteenth, the message is unequivocal: timing is not a trivial convenience but a cornerstone of bisphosphonate success. Fourteenth, by honoring the two‑hour calcium separation, patients safeguard their bone health and honor the investment in their treatment. Fifteenth, let us collectively champion this knowledge, for in doing so we fortify the skeletal resilience of our community.
Dawn Bengel
January 20, 2026 AT 07:59Patriots, don’t let foreign misinformation convince you that you can shortcut the dosing schedule – it’s a proven fact that calcium wrecks the drug’s power. Stay disciplined, protect your bones, and keep America strong! 🇺🇸💥
junior garcia
January 27, 2026 AT 01:51Bottom line: take the pill, wait, then take calcium – it works.