Antacids and Antibiotics: How to Time Your Doses to Avoid Treatment Failure
 Nov, 14 2025
Nov, 14 2025
When you’re on antibiotics and your stomach starts acting up, it’s tempting to grab an antacid. Tums, Rolaids, Maalox - they’re right there on the shelf, and they promise quick relief. But if you take them at the same time as your antibiotic, you might be sabotaging your treatment. This isn’t just a myth. It’s a well-documented, clinically significant interaction that can cut antibiotic effectiveness by up to 90% - and leave you with a lingering infection you thought was under control.
Why Antacids Mess With Antibiotics
Antacids work by neutralizing stomach acid. That’s great for heartburn. But your body needs a certain level of acidity to absorb some antibiotics properly. More importantly, antacids containing aluminum, magnesium, or calcium don’t just reduce acid - they chemically bind to certain antibiotics. This binding forms a compound your gut can’t absorb. It’s like putting a lock on the antibiotic and throwing away the key.
That’s called chelation. It’s not guesswork. Studies show magnesium trisilicate can reduce tetracycline absorption by half. Ciprofloxacin, a common fluoroquinolone antibiotic, sees up to 90% less absorption when taken with antacids. That means if you’re treating a UTI or pneumonia with ciprofloxacin and you take it with Tums, you might as well be taking sugar pills.
It’s not just about chelation. Antacids also raise your stomach’s pH. Antibiotics like doxycycline need an acidic environment to dissolve and enter your bloodstream. When you neutralize the acid, the drug doesn’t break down right. The result? Less medicine reaches your infection.
Which Antibiotics Are Most Affected?
Not all antibiotics are equally vulnerable. Some are barely touched by antacids. Others? They’re extremely sensitive.
High-risk antibiotics:
- Ciprofloxacin, levofloxacin, moxifloxacin - Fluoroquinolones. These are the most affected. Absorption drops by 75-90% with antacids. The NHS and FDA both require clear labeling: take these antibiotics at least 2 hours before or 4 hours after antacids.
- Doxycycline, tetracycline - Tetracycline-class antibiotics. These lose 50-70% of their effectiveness when taken with antacids. Even a small delay helps. Take them 2-3 hours apart.
Moderate-risk antibiotics:
- Amoxicillin, cephalexin - Penicillins and cephalosporins. These are less affected, but still show a 15-20% drop in absorption. It’s not dangerous, but it’s not ideal. A 1-2 hour gap is enough.
Low-risk antibiotics:
- Azithromycin, clarithromycin - Macrolides. Minimal interaction. Still, 2 hours separation is recommended as a safety buffer.
- Metronidazole - No known interaction. You can take this with antacids without timing issues.
Here’s the bottom line: if your antibiotic is a fluoroquinolone or tetracycline, timing isn’t optional. It’s essential.
What About H2 Blockers and PPIs?
Many people switch from antacids to famotidine (Pepcid) or omeprazole (Prilosec) thinking they’re safer. And they are - but not because they’re harmless. They’re safer because they don’t contain aluminum, magnesium, or calcium. They work differently. They reduce acid production over time instead of instantly neutralizing it.
Studies show that switching from antacids to PPIs or H2 blockers cuts treatment failure rates in half. One 2023 study found that patients on antibiotics who switched from Tums to omeprazole dropped their treatment failure rate from 27% to just 9%. That’s a massive difference.
Still, even PPIs can slightly reduce absorption of some antibiotics like ketoconazole or itraconazole. But for most common antibiotics - including ciprofloxacin and doxycycline - they’re a much better choice than antacids if you need long-term acid control.
Real-World Consequences
This isn’t theoretical. Real people are getting sicker because they don’t know how to time their meds.
On Reddit, a physician shared that five patients in one year had recurring UTIs - all because they took ciprofloxacin with Tums. Once they spaced the doses by four hours, the infections cleared. On WebMD, 68% of patients who reported antibiotic failure said their symptoms went away only after they fixed their timing.
It’s not just patients. Doctors see it too. A 2022 survey of 1,200 primary care physicians found that 18% of apparent antibiotic failures were due to improper antacid timing. That’s nearly one in five cases where the patient took the right drug - but at the wrong time.
The CDC estimates that 15% of emerging fluoroquinolone resistance is linked to subtherapeutic antibiotic levels caused by these interactions. That means improper timing isn’t just causing one failed treatment - it’s helping create superbugs.
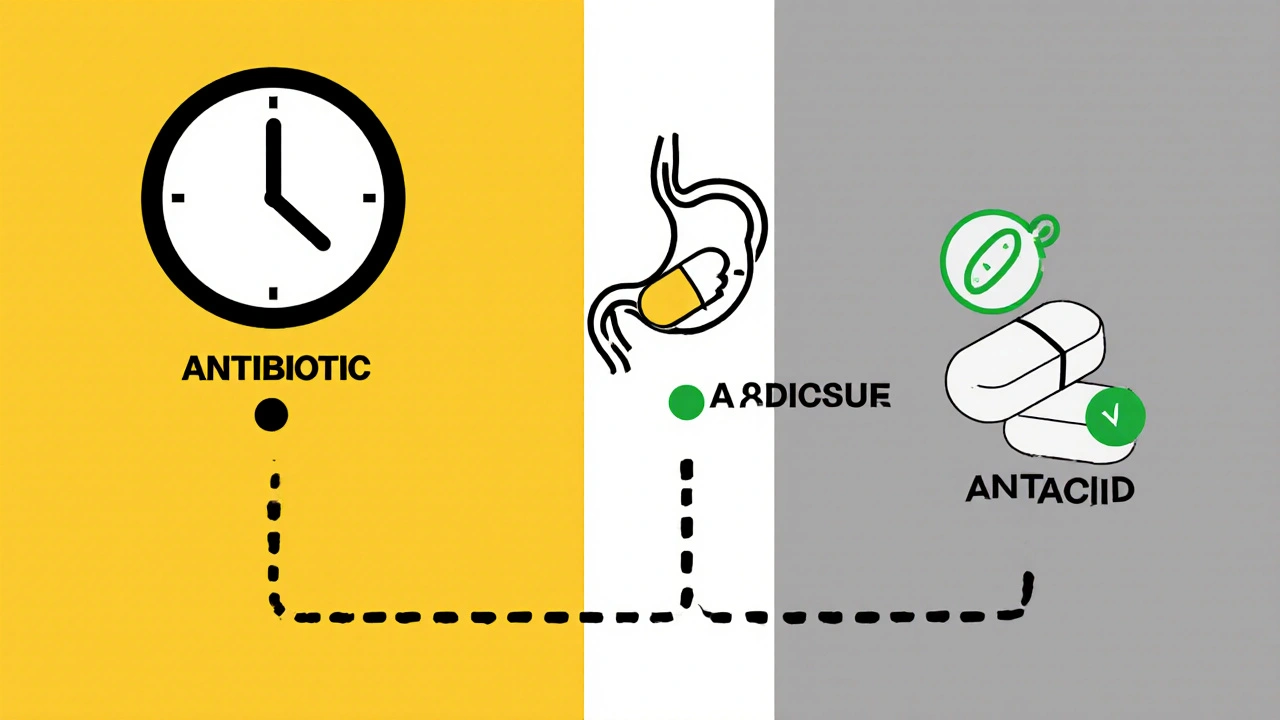
How to Get the Timing Right
Let’s cut through the confusion. Here’s what you actually need to do:
- Know your antibiotic. Is it ciprofloxacin? Doxycycline? Then timing matters. Is it amoxicillin? Metronidazole? Less critical, but still better to separate.
- Use the 2-4 hour rule. For fluoroquinolones: wait 4 hours after taking an antacid before taking your antibiotic. Or take the antibiotic 2 hours before the antacid. For tetracyclines: 2-3 hours apart. For others: 1-2 hours.
- Plan your day. If you take your antibiotic in the morning, take your antacid at night. Or vice versa. Avoid taking both with meals - meals already delay absorption. Add antacids into the mix, and you’re asking for trouble.
- Use a reminder app. Apps like MyMedSchedule have built-in alerts for antacid-antibiotic conflicts. They’ll tell you when to take each one. Set them up. It takes two minutes.
- Ask your pharmacist. They’re trained to catch these things. If you’re unsure, don’t guess. Ask.
Pro tip: If you’re on antibiotics for acne (like doxycycline), don’t take your antacid right after breakfast. Wait until after lunch or dinner. That’s a simple shift that makes a huge difference.
What If You Already Took Them Together?
Did you accidentally take ciprofloxacin with Tums? Don’t panic. One mistake won’t ruin your whole course. But don’t repeat it.
If you realize right away - within 30 minutes - you can try taking another dose of the antibiotic. But only if your doctor says it’s safe. Don’t double up without checking. If it’s been more than an hour, skip the extra dose. Just space the next one properly.
The key is consistency. One slip-up won’t kill you. But doing it every day? That’s how treatment fails.
What’s Changing in 2025?
The FDA approved a new version of ciprofloxacin in 2023 called Cipro XR-24. It’s designed to release slowly and resist chelation. In trials, it only lost 8% of its absorption when taken with antacids - compared to 90% for the old version. It’s not widely available yet, but it’s a sign of where things are headed.
Also, in 2023, the American Society of Health-System Pharmacists updated guidelines to distinguish between antacid types. Calcium-based antacids (like Tums) require longer separation than magnesium-based ones (like Milk of Magnesia). That’s new. It means your pharmacist might now give you more precise advice than before.
And in the future? Genetic testing may tell you how fast your stomach empties. That could lead to personalized timing - not just “2 hours apart,” but “take it 1.5 hours before your antacid because your body processes it faster.”
Final Takeaway
You’re not being lazy if you forget to space your meds. You’re just not told how important it is. Most people assume if the pill is in their mouth, it’s working. But with antibiotics and antacids, timing is everything.
If you’re on ciprofloxacin or doxycycline, treat the antacid like a rival drug - not a helper. Separate them by hours, not minutes. Use apps. Ask your pharmacist. Switch to PPIs if you need daily acid control.
It’s not complicated. But it’s critical. Get it right, and your infection clears. Get it wrong, and you’re not just wasting time - you’re risking more serious illness, longer recovery, and even contributing to antibiotic resistance.
One simple habit - waiting a few hours - can mean the difference between feeling better in a week… or being back in the doctor’s office next month.
Can I take antacids with amoxicillin?
Yes, but not at the same time. Amoxicillin is less affected than antibiotics like ciprofloxacin or doxycycline, but studies show it still absorbs 15-20% less when taken with antacids. To be safe, wait at least 1-2 hours between doses. If you’re on amoxicillin and only need antacids occasionally, take them after dinner and your antibiotic in the morning.
How long should I wait after taking an antacid before taking my antibiotic?
It depends on the antibiotic. For fluoroquinolones like ciprofloxacin, wait 4 hours after taking an antacid. For tetracyclines like doxycycline, wait 2-3 hours. For most others, including amoxicillin or azithromycin, 1-2 hours is enough. If you’re unsure, aim for 4 hours - it’s safe for all types.
Is it okay to take antacids before my antibiotic?
Yes - and sometimes it’s better. For fluoroquinolones, taking the antibiotic 2 hours before the antacid is just as effective as waiting 4 hours after. This can be easier to fit into your schedule. For example, take your antibiotic at 7 a.m., then your antacid at 9 a.m. Just make sure you stick to the window - don’t take them closer than 2 hours apart.
What’s the best antacid to use with antibiotics?
The best choice isn’t an antacid at all - it’s a PPI like omeprazole or an H2 blocker like famotidine. These don’t contain aluminum, magnesium, or calcium, so they don’t cause chelation. If you need daily acid relief while on antibiotics, switching to one of these reduces treatment failure risk by more than half. Save antacids for occasional use only.
Can I drink milk or eat dairy with my antibiotic if I’m taking antacids?
Milk and dairy contain calcium, which can also bind to antibiotics like tetracyclines and fluoroquinolones. So if you’re already taking an antacid with calcium, adding milk makes it worse. Avoid dairy for at least 2-4 hours around your antibiotic dose - same as you would with antacids. Stick to water when taking your antibiotic unless your doctor says otherwise.

Rachel Wusowicz
November 15, 2025 AT 16:14So... you're telling me the government AND Big Pharma are secretly using antacids to weaken antibiotics so we get sicker and need MORE prescriptions? I've been taking Tums with my doxycycline for years... and now I'm wondering if my chronic fatigue, brain fog, and that weird rash were all part of a coordinated suppression campaign. They know we're vulnerable. They know we trust our meds. They let us take them together. It's not negligence-it's design.
ZAK SCHADER
November 16, 2025 AT 02:59Yall got too damn soft. Back in my day we just swallowed pills with a beer and called it good. Now you need a fucking schedule and apps? Just take the damn antibiotic and shut up. If it don't work, go to the ER. That's what insurance is for.
Danish dan iwan Adventure
November 16, 2025 AT 10:16Chelation kinetics are non-linear. Calcium-based antacids exhibit higher binding affinity for fluoroquinolones due to ionic radius compatibility. Optimal separation window: 4h post-antacid for Cipro. PPIs preferred for chronic use. QED.
Ankit Right-hand for this but 2 qty HK 21
November 16, 2025 AT 12:59Who even uses Tums anymore? That's a 1990s grandma solution. If you're that desperate for acid relief you're already doing something wrong. Take a cold shower. Stop eating junk. Or better yet-move to India where we don't need pills to digest McDonald's.
Oyejobi Olufemi
November 16, 2025 AT 20:25Listen… I’ve studied this. Not just read it. I’ve sat in silence with my gut for 7 days, fasting, meditating, listening to the whispers of the microbiome. You think it’s about timing? No. It’s about ENERGY. Antacids disrupt your body’s natural electromagnetic field. Antibiotics? They’re synthetic vibrations. When you combine them… your soul’s frequency gets scrambled. That’s why you feel tired. That’s why you relapse. You’re not fighting bacteria-you’re fighting cosmic interference. And the FDA? They know. They’re silent because they’re part of the matrix.
Latrisha M.
November 17, 2025 AT 16:46If you're on cipro or doxycycline, just wait 4 hours between antacids and antibiotics. It’s simple. Use a phone alarm. Or write it on your hand. Don’t overthink it. Your body will thank you.
Jamie Watts
November 18, 2025 AT 04:57Bro I took cipro with Tums like 3 times last week and I’m fine. You guys act like this is nuclear physics. I’ve had UTIs 5 times and I’m still standing. Maybe your body just works different. Or maybe you’re just scared of your own stomach
John Mwalwala
November 19, 2025 AT 01:07Did you know that aluminum in antacids can bioaccumulate in the brain? And when it binds to ciprofloxacin? That complex can cross the blood-brain barrier. That’s why people on long-term antibiotics + antacids report memory loss, tinnitus, even hallucinations. It’s not coincidence. It’s pharmacokinetic synergy. I’ve seen the peer-reviewed studies. The CDC buried them. They don’t want you to know your meds are slowly poisoning your neurons.
Deepak Mishra
November 20, 2025 AT 20:02OMG I JUST REALIZED I TOOK MY CIPRO WITH TUMS THIS MORNING 😭😭😭 I’M GONNA DIE FROM SUPERBUGS NOW 😭😭😭 I’M SO STUPID I CAN’T EVEN TAKE PILL RIGHT 😭😭😭 I’M GONNA BE A LAB RAT FOR THE CDC 😭😭😭
Diane Tomaszewski
November 22, 2025 AT 18:14I used to take antacids with everything. Then I started spacing them out. My stomach didn’t magically heal. But my infection cleared on time. Sometimes the simplest things work best.
Dan Angles
November 24, 2025 AT 03:12It is imperative that patients adhere to the temporal separation protocols delineated in current clinical guidelines. Failure to do so constitutes a deviation from standard of care and may result in therapeutic suboptimization. Pharmacists are uniquely positioned to mitigate this risk through patient counseling and medication reconciliation.
David Rooksby
November 24, 2025 AT 20:20Okay so here’s the thing - I’ve been on antibiotics for a month now because my doctor kept prescribing different ones, and I thought it was because I was ‘resistant’ - turns out I was just taking antacids with my doxycycline after every meal because I ate too much curry. I didn’t know calcium was in Tums - I thought it was just ‘chalk’. Now I’ve got this app that pings me every time I try to take them together. I’m not a genius. I’m just a guy who didn’t know. And now I’m trying to unlearn everything I thought I knew about my own body. It’s embarrassing. But I’m learning.
Melanie Taylor
November 25, 2025 AT 22:24PSA: If you’re on antibiotics and you feel bloated, try ginger tea instead of Tums. It’s natural, helps digestion, and doesn’t mess with your meds 😊
Teresa Smith
November 27, 2025 AT 12:10This isn’t about being perfect. It’s about being aware. One mistake doesn’t doom you. But repeating it? That’s where the danger lives. You’re not failing because you forgot. You’re failing because you didn’t know it mattered. Now you know. That’s progress.
Daniel Stewart
November 29, 2025 AT 10:30Perhaps the real issue isn't the antacid, but the cultural assumption that pharmaceuticals are inert, passive agents - that their efficacy is purely chemical, and not relational. We treat our bodies like machines, and our drugs like tools. But the body is a conversation, not a circuit. Timing, rhythm, context - these are not technicalities. They are the grammar of healing.